- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Genetic insights improve tumor classification
Author(s):
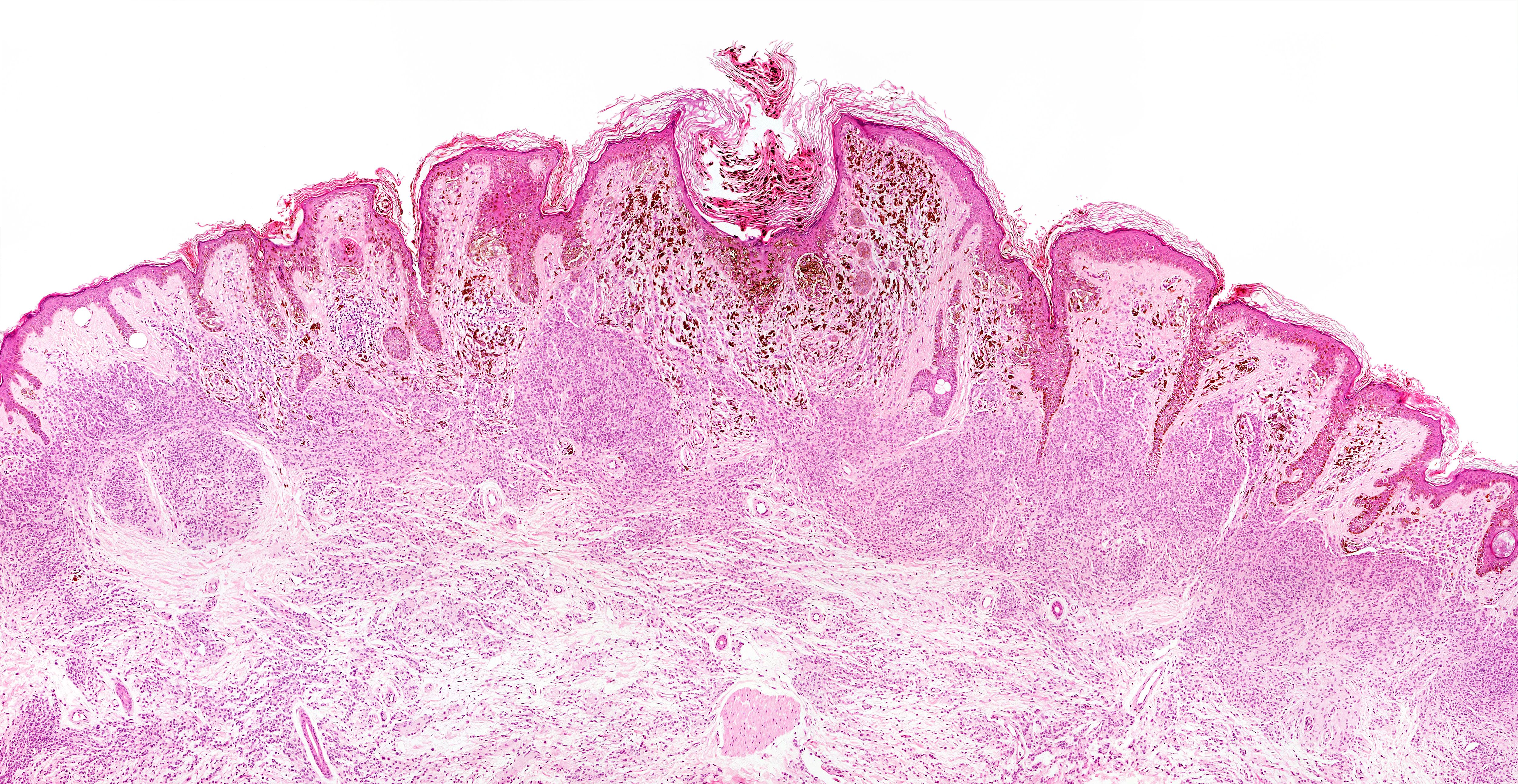
Accurately diagnosing some melanocytic neoplasms is challenging because they may fall into a grey area histologically, one expert says. Recent progress in molecular genetics can help dermatopathologists more precisely classify tumors, leading to more appropriate treatment and management choices.
“We are now trying to identify the genetic differences between these intermediate tumors and their more malignant counterparts and studying long-term outcomes to guide patient management,” Dr. Yeh says. (Convit - stock.adobe.com)
Dr. Yeh

Accurately diagnosing some melanocytic neoplasms is challenging because they may fall into a grey area histologically, one expert says. These can create disagreement even between the most experienced dermatopathologists.
While some view classifying a melanocytic tumor as intermediate or borderline as indecisiveness, recent progress in molecular genetics has demonstrated that there really is an intermediate or borderline category of melanocytic tumor, corresponding to difficult-to-classify melanocytic lesions, says Iwei Yeh, M.D., Ph.D., associate professor of dermatology, department of dermatology, University of San Francisco School of Medicine, San Francisco, Calif., who recently spoke at the World Congress of Dermatology in Milan.
The recognition of intermediate and borderline tumors helps clinicians and dermatopathologists more precisely classify tumors leading to more appropriate treatment and management choices for this patient population.
“Not being able to classify every tumor as clearly benign or malignant does not reflect an inability of dermatopathologists to agree on the right classification, because we now know that there really is a spectrum of tumors with some falling in intermediate categories. It has been really interesting to demonstrate that there are melanocytic tumors that have characteristic histopathologic features and very specific combinations of genetic mutations,” Dr. Yeh says. Melanocytic neoplasms consist of a group of several different tumor types that are categorized by a number of distinct clinical, pathological and genetic features, and the clinical course of these tumors may be indolent (i.e., benign nevi), aggressive (i.e., malignant melanoma), or intermediate (i.e., melanocytic tumors of uncertain malignant potential), Dr. Yeh explains.
Spitz tumors are a group of melanocytic tumors that have distinctive histologic features, and include benign tumors (i.e., Spitz nevi), malignant tumors (i.e., Spitzoid melanoma), and tumors with borderline histopathologic features and uncertain clinical outcome (i.e., atypical Spitz tumors).
“Any given nevus likely has only a single genetic mutation that initiates its growth whereas melanomas have accumulated a number of genetic mutations. Now we know that there is actually a class of tumors that have more mutations than nevi but are not malignant,” Dr. Yeh says.
As a result of this new genetic information, melanocytic tumors such as Spitz nevi, common acquired nevus, BAP1-inactivated Spitzoid nevi, and deep penetrating nevus are not only being newly classified but are also changing the general understanding of why certain types of intermediate tumors occur.
According to Dr. Yeh, genetics can now elucidate many of the past ambiguities concerning the benign or malignant nature of questionable lesions such as atypical Spitz tumor and deep penetrating nevus and has confirmed that intermediate tumors should be separately categorized.
Nevertheless, it can still be sometimes challenging for dermatopathologists to accurately classify intermediate tumors by histopathologic features alone, and molecular testing can help stratify melanocytic tumors, Dr. Yeh says.
“We are now trying to identify the genetic differences between these intermediate tumors and their more malignant counterparts and studying long-term outcomes to guide patient management,” Dr. Yeh says.
Different types of melanocytic tumors have different genetic alterations and therefore also develop along distinct pathways. Now that an intermediate melanocytic tumor type has been established, one future challenge dermatopathologists will face is refining their ability to categorize tumors and stratify them with respect to risk, for which there is no clear consensus yet.
The newly published WHO Classification of Tumors began to take genetic classifications into account when categorizing tumors, indicating that it is becoming accepted that genetic features can help dermatopathologists more accurately classify tumors into categories such as blue nevus, common acquired nevus, and Spitz nevus. According to Dr. Yeh, this can help clinicians better assess the malignant potential of tumors as well as their appropriate treatment and management.
“It is now clear that there are different subclasses of melanocytic tumors each of which encompasses a continuum from benign to malignant. It has been really nice to see that genetics has now validated much of the work that was done by dermatopathologists in defining subtypes of melanocytic tumors as we now know these subtypes reflect distinct genetics,” Dr. Yeh says. Â
Disclosures:
Dr. Yeh reports no relevant disclosures.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.















