- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Nanovaccine shows promise for melanoma
Author(s):
A novel nanovaccine has demonstrated efficacy in preventing the development of melanoma in mouse models, according to a recent study.
“The nanoparticles ... stimulated the immune system of the mice, and the immune cells learned to identify and attack cells containing the two peptides, that is, the melanoma cells," says Prof. Ronit Satchi-Fainaro.
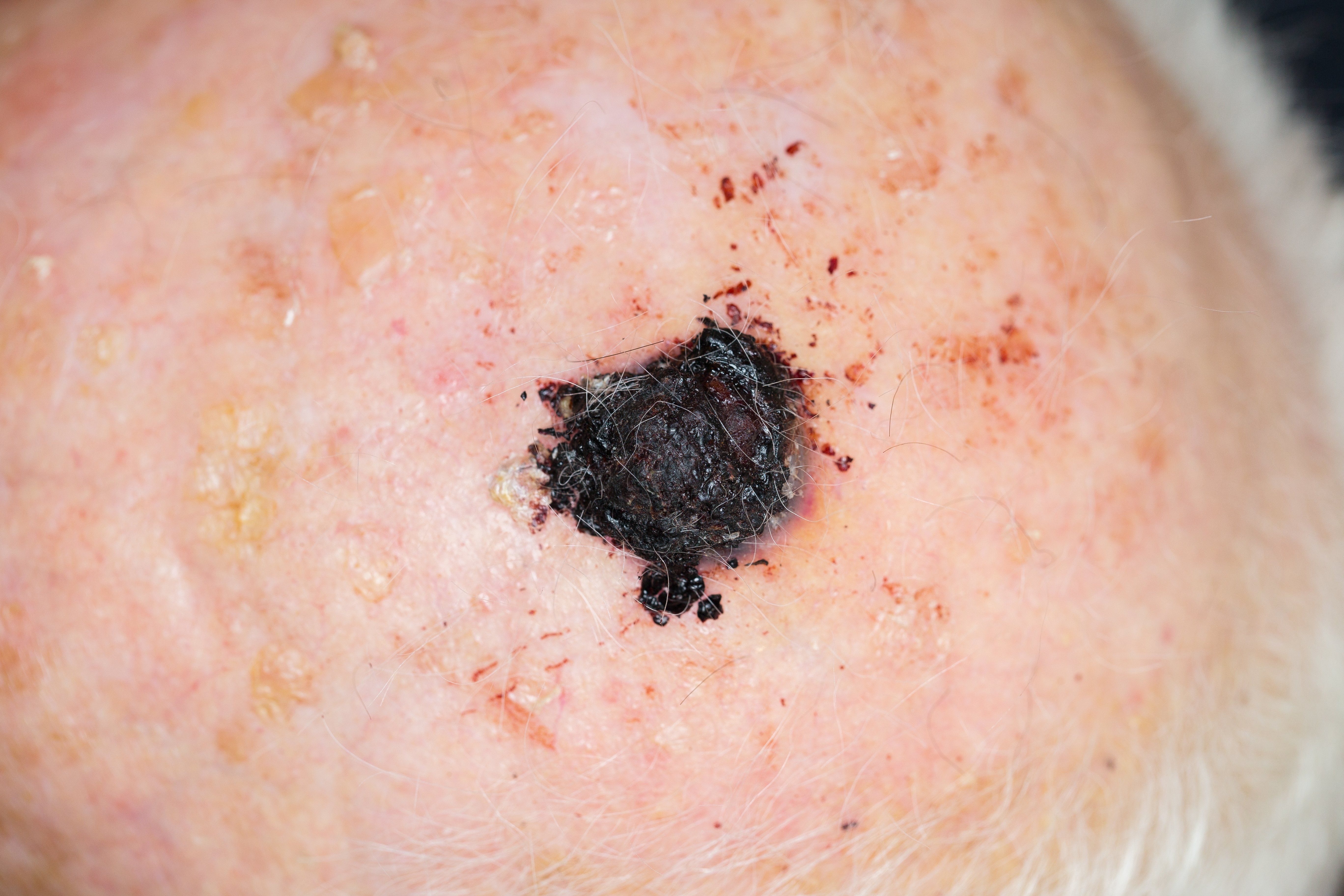
A novel nanovaccine has demonstrated efficacy in preventing the development of melanoma in mouse models, as well as in treating primary tumors and metastases that result from melanoma.1 This breakthrough could pave the way for a truly effective melanoma vaccine approach that may even prove useful in the most advanced stages of the disease.
RELATED: Technology improves histologic diagnosis in melanoma
“In our study, we have shown that it is possible to produce an effective nanovaccine against melanoma and to sensitize the immune system to immunotherapies,” says Prof. Ronit Satchi-Fainaro, chair of the department of physiology and pharmacology and head of the Laboratory for Cancer Research and Nanomedicine at Tel Aviv University Sackler Faculty of Medicine, Tel Aviv, Israel, who co-led the research.
In a collaborative effort between Prof. Satchi-Fainaro’s team and fellow colleagues from the Research Institute for Medicines (iMed.ULisboa), faculty of pharmacy, Universidade de Lisboa, Lisbon, researchers developed a clever nanovaccine for melanoma that achieved impressive therapeutic outcomes in mice.
After harnessing tiny particles of approximately 170 nanometers in size, made of biodegradable polymer, they packed each particle full with two peptides, or short chains of amino acids, that are also expressed in melanoma cells. The nanoparticles or “nanovaccine” were then injected in a mouse model bearing melanoma.
RELATED: Melanoma management perspectives vary
“The nanoparticles acted just like known vaccines for viral-borne diseases. They stimulated the immune system of the mice, and the immune cells learned to identify and attack cells containing the two peptides, that is, the melanoma cells. This meant that, from now on, the immune system of the immunized mice will attack melanoma cells if and when they appear in the body,” Prof. Satchi-Fainaro says.
The nanovaccine was tested under various conditions and was found to be effective in preventing the development of melanoma, delayed the progress of the disease, and appeared to work in preventing or slowing brain metastases. Researchers injected healthy mice with the nanovaccine, and then melanoma cells, upon which the mice remained healthy.
RELATED: Head and neck melanoma characteristics
A combination of the vaccine and immunotherapy treatments was also used to treat the primary tumor. Results showed that the synergistic effect of the combination therapy significantly delayed the progression of the disease and greatly extended the lives of all treated mice. The researchers also validated their approach on tissues taken from patients with melanoma brain metastases, suggesting that the nanovaccine can be used to treat brain metastases as well.
Advances in immune therapy for melanoma have improved treatment outcomes based on antitumor immune responses elicited by the patient’s own immune system. However, a low response rate, acquired resistance and severe side effects have limited the clinical outcomes of immune checkpoint therapy. With the clinical successes achieved with CTLA-4 (cytotoxic T-lymphocyte-associated protein-4) and PD-1 (programmed cell death protein 1) blockade in enhancing specific T-cell-mediated antitumor immunity, efforts have now been made to stimulate the signaling pathways of the immune system.
“The war against cancer in general, and melanoma in particular, has advanced over the years through a variety of treatment modalities, such as surgery, chemotherapy, radiation therapy and immunotherapy; but the vaccine approach, which has proven so effective against various viral diseases, has not materialized yet against cancer,” Prof Satchi-Fairnaro says.
RELATED: Genetic test could rule out melanoma diagnosis
“Our research opens the door to a completely new approach – the vaccine approach – for effective treatment of melanoma, even in the most advanced stages of the disease. We believe that our platform may also be suitable for other types of cancer and that our work is a solid foundation for the development of other cancer nanovaccines,” Prof. Satchi-Fainaro concludes.
References:
1. Conniot J, Scomparin A, Peres C, Yeini E, Pozzi S, et al. Immunization with mannosylated nanovaccines and inhibition of the immune-suppressing microenvironment sensitizes melanoma to immune checkpoint modulators. Nat Nanotechnol. 2019 Sep;14(9):891-901. doi: 10.1038/s41565-019-0512-0. Epub 2019 Aug 5.















