- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
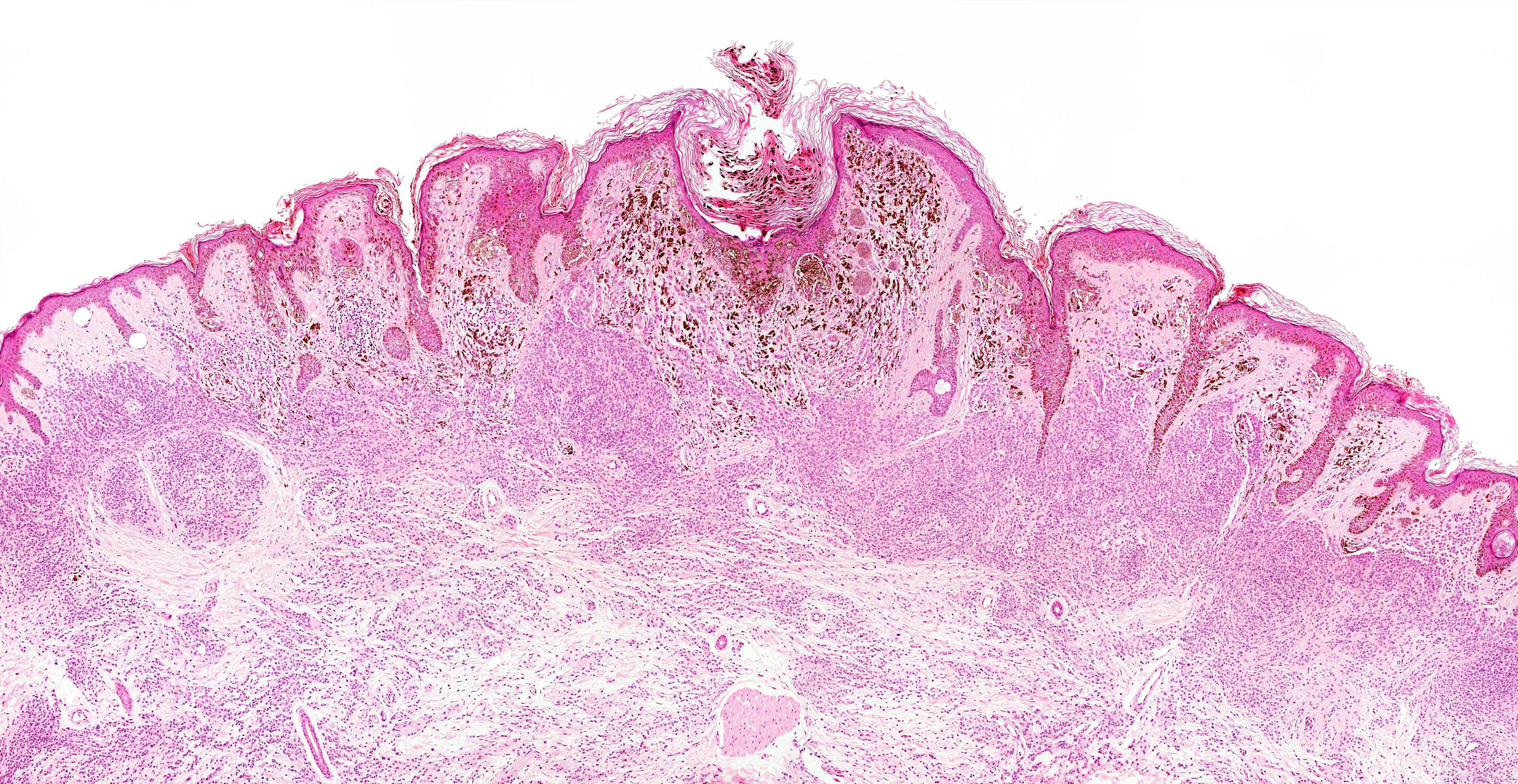
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Pulsed dye laser may improve nonvascular conditions
Author(s):
The 595 nm pulsed dye laser (PDL) may provide an e ffective option for nonvascular conditions, such as scars, acne and molluscum contagiosum, according to a recent review.

Dr. Graber

The 595 nm pulsed dye laser (PDL) may provide an effective option for nonvascular conditions, such as scars, acne and molluscum contagiosum, according to a recent review. However, evidence from large, randomized controlled trials makes drawing firm conclusions difficult.
RELATED: Oxymetazoline, pulsed dye laser show promise for rosacea
Researchers led by Emily Forbat, MBBS, of the dermatology unit at Warwick Hospital in Warwick, U.K., reviewed a total of 84 studies and concluded that PDL has demonstrated efficacy in acne, scar remodeling and prevention, post-filler bruising, nail psoriasis, low-risk basal cell carcinoma and warts.1 Some studies, however, showed no significant differences between PDL and more conventional regimens. Additionally, variable results have emerged in plaque psoriasis. The review appeared online in April 2019 in the Journal of Cosmetic Dermatology.
“While the review is a good collection and summarization of a lot of studies,” says Emmy Graber, M.D., MBA, who was not involved with the study, “there’s a paucity of large-scale, randomized, controlled studies looking at the pulsed dye laser for nonvascular indications. So it’s very hard to draw conclusions from this study.” She is president of the Dermatology Institute of Boston and an a liate clinical instructor at Northeastern University.
Forbat et al. reviewed 12 acne studies, but these studies included fewer than 400 patients total. Among the indications reviewed, Dr. Graber is most familiar with PDL in acne.
“And there are a lot of studies out there. But they’re all small, and they have varying conclusions. Often different parameters or settings are used on the pulsed dye laser. So, you can’t compare one to another,” she says.
Ideally, she says, someone would perform a large split-face study of PDL in acne; however, it’s hard to conduct blinded laser studies.
RELATED: Energy-based options for acne
On a broader scale, she says that despite the commonality of acne, there’s still no ideal, widely studied and accepted treatment.
“And it seems that patients increasingly are seeking alternative treatments aside from the traditional prescription creams and pills,” she says. “They are inquiring about lasers or other treatment modalities for acne. It would be great if we had a really sound study that we could base some conclusions on. However, we don’t. Some studies included in the manuscript showed that the pulsed dye laser helps acne; some showed that it didn’t.”
For example, a 30-patient split-face study showed that two sessions twice weekly for eight weeks produced no significant improvement over no treatment at all.2
For scarring, the review included studies that compared PDL to other lasers and light sources including erbium, fractional CO2, KTP, Nd:YAG, low-level laser and intense pulsed light (IPL), along with botulinum toxin. While all treatment modalities demonstrated improvement in scar outcomes, write Forbat et al., most studies showed no significant improvement between treatment arms.
Nevertheless, Dr. Graber says that by including 23 scar studies, the paper reflects the clinical reality that scarring is the most frequent nonvascular indication for which dermatologists use PDL.
RELATED: Topical cantharidin for molluscum
“We know that there are some other types of lasers that work as well. But this paper further emphasizes that the pulsed dye laser is an effective means for treating scars. That’s one of the sound conclusions that can be drawn.”
Molluscum lesions are often difficult to treat, she says. There’s no ideal therapy in that many of the treatment approaches either hurt or leave scars. Utilizing the pulsed dye laser is an interesting approach and worth considering if a patient fails or is not a candidate for other therapies. However, the review does not support a conclusion that PDL should be first-line treatment, she adds.
Outcomes varied when treating striae. One study showed slight improvement in treating mature striae twice monthly for up to two years; another found that both PDL and IPL improved the appearance of striae, and that early striae rubra (SR) fared better with both treatments. In the latter study, PDL was found to significantly increase collagen 1 expression versus IPL.3 Forbat et al. say this difference could make PDL preferred if larger studies support this finding.
Dr. Graber says, “My big takeaway from this paper is that the pulsed dye laser can be used for many different dermatologic conditions. But it’s best used in the indications for which it’s tried and true, such as erythema, telangectasias, rosacea and port wine stains.”
Disclosures:
Dr. Graber has received research funding from Sebacia.
References:
1. Forbat E, Al-Niaimi F. Nonvascular uses of pulsed dye laser in clinical dermatology. J Cosmet Dermatol. 2019Apr 19. doi: 10.1111/jocd.12924. [Epub ahead of print]
2. Lekwuttikarn R, Tempark T, Chatproedprai S, et al. Controlled trial split-faced study of 595-nm pulsed dye laser in the treatment of acne vulgaris and acne erythema in adolescence and early adulthood. Int J Dermatol. 2017;56:884-888.
3. Shokeir H, El Bedewi A, Sayed S, et al. Effi cacy of pulsed dye laser versus intense pulsed light in the treatment of striae distensae. Dermatol Surg. 2014;40:632-640.