- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
2011 Medicare physician fee schedule appears positive for dermatologists
The 2011 Medicare physician fee schedule published Nov. 29 by the Centers for Medicare & Medicaid Services (CMS) offers valuable insight into reimbursement for 2011. The final rule adjusts work relative value units downward for many services, but dermatology emerges as one of winners, getting a 4 percent increase overall.

Key Points

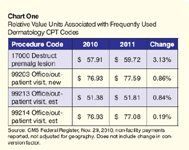
The final rule adjusts work relative value units (wRVUs) downward for many services, but dermatology emerges as one of winners, getting a 4 percent increase overall, according to the CMS estimates published in the final rule (see Chart One for changes to frequently used codes). This is because a higher proportion of the specialty's payments are based on practice expense RVUs.
In its press release following the reversal of the reimbursement cut, the American Medical Association expounds: "Many physicians made (it) clear that this year's roller coaster ride, caused by five delays of this year's cut, forced them to make difficult practice changes like limiting the number of Medicare patients they could treat."
The government also stepped in to halt the 23 percent cuts that were scheduled to take effect on Dec. 1, 2010. The government's action froze current 2010 rates for services provided to Medicare beneficiaries through the end of the year. The 31-day "patch" is being funded through the $1 billion gain from the 20 percent cut in payments for outpatient therapy services.
Improvement initiatives
The Nov. 29 rule also finalizes several details of CMS' physician fee initiatives for electronic prescribing and claims-based reporting on quality. The latter initiative, the Physician Quality Reporting Initiative (PQRI), is the government's pay-for-performance program. In 2011, it will pay 1 percent of total allowed charges to those who successfully participate.
The welcome news is that CMS will decrease the sample reporting requirement from 80 percent to 50 percent of Medicare patients next year for physicians who report on a claims basis. In other words, claims-based reporting participants are still required to select three measures to report, but they only need to report on 50 percent - versus 80 percent in previous years - of the Medicare patients who qualify for those measures.
CMS expands the number of individual measures by 20 in 2011 and will allow practices with two or more physicians to participate in PQRI as a "group." Formerly, group participation was limited to practices with more than 200 physicians.
CMS also confirmed that incentive payments of 0.5 percent of annual Medicare reimbursement are authorized for years 2012 through 2014, while a penalty in the form of a decrease of Medicare payments for PQRI nonparticipants will commence in 2015.
Also new in the final rule is an additional 0.5 percent payment to physicians who attest to successfully participate in an American Board Medical Specialties–qualified maintenance of certification program (MOCP) during 2011, with the bonus extending through 2014. CMS defines an MOCP, or an equivalent program, as one that advances quality, lifelong learning and self-assessment of board-certified specialty physicians.
The Maintenance of Certification-Dermatology (MOC-D) created and administered by the American Board of Dermatology would qualify because it focuses on practice-based learning and enhancement of competencies such as patient care, medical knowledge, professionalism and communications skills. The MOC-D is a 10-year cycle consisting of components that evaluate the board-certified dermatologist's cognitive expertise and practice performance among other factors.
Another welcome change coming to PQRI in 2011 is the introduction of a feedback loop, of sorts. CMS has faced sharp criticism from physicians who participated in PQRI but received no bonus payment. Physicians complained that they were given no opportunity to learn what they needed to correct in time to qualify.
For 2011, CMS says it will provide feedback within 60 days to those who e-mail their PQRI questions to qnetsupport@sdps.org
or call the help desk at (866) 288-8912. Visit http://www.cms.gov/pqri/ for more information.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.
















