- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Acne in skin of color
Author(s):
Skin of color patients exhibit clinical and therapeutic nuances that affect acne management. Dermatologists should understand how these patients present, clinically; how to treat them safely; cultural factors; and their specific desired treatment endpoints.
vulgaris is the leading dermatologic diagnosis among the population of Americans collectively referred to as people with skin of color: African Americans, Hispanics/Latinos and Asians/Pacific Islanders.1 Dermatologist Andrew F. Alexis, M.D., M.P.H., who reported that finding in the June 2014 Journal of Drugs in Dermatology, also conducted a comparative study at his Skin of Color Center in New York City and found that acne was the leading diagnosis in African Americans, Hispanic/Latinos and Caucasians.2
Skin of color patients exhibit clinical and therapeutic nuances that affect acne management. Dermatologists should understand how these patients present, clinically; how to treat them safely; cultural factors; and their specific desired treatment endpoints, according to Dr. Alexis.
Dr. Alexis, who is dermatology chair at Mount Sinai St. Lukes and Mount Sinai Roosevelt, New York, N.Y., presented on acne and rosacea in skin of color, during the May 2015 Skin of Color Seminar in New York City


Keloid scarring on the chest
Photo credit: Andrew F. Alexis, M.D.
NEXT: What dermatologists should know
What dermatologists should know

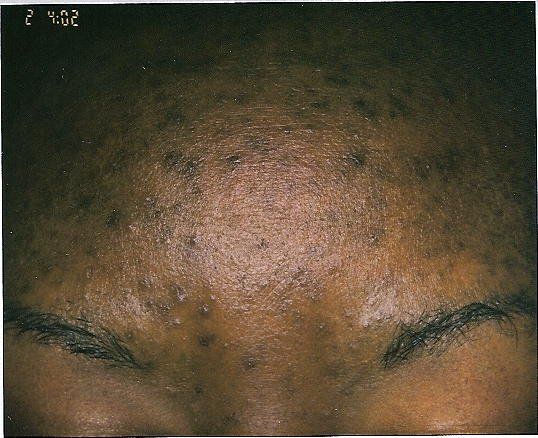

Acne with postinflammatory hyperpigmentation
Photo credit: Andrew F. Alexis, M.D.
These are distinct features of acne in patients with skin of color, according to Dr. Alexis: Skin of color acne patients have a tendency to develop postinflammatory hyperpigmentation, which is frequently of equal or greater concern to the patient as the acne, itself.
They have a higher risk than Caucasian patients of keloids or hypertrophic scars, arising at sites of moderate-to-severe acne. The scars are especially likely on the chest and back.
READ: Many acne patients do not get all their meds
Cultural practices in patients with skin of color may increase acne risk. Many African Americans, for example, use of hair products that contain oils, which can be comedogenic and produce “pomade acne,” he said. Another example: the use of cocoa butter is common practice among African Americans, who hope to improve their complexions.
“[There is a] widely held but unproven belief that cocoa butter evens the skin tone,” Dr. Alexis said. “This can, in turn, exacerbate acne because of its comedogenic nature.”
NEXT: Latest research findings
Latest research findings



Acne with postinflammatory hyperpigmentation
Photo credit: Andrew F. Alexis, M.D.
Because of higher risks of pigmentary abnormalities among patients with skin of color, dermatologists should evaluate the safety of topical acne products that might irritate the skin, before recommending patients use them, Dr. Alexis said. “Fortunately, there have been studies of the major topical agents that have specifically looked at tolerability and overall safety in patients with higher Fitzpatrick types. These include recent studies of adapalene 0.1%-benzoyl peroxide 2.5% gel in black patients3… and dapsone gel, 5% in adult skin of color females with facial acne vulgaris, which was presented at the Skin of Color Seminar Series annual meeting,” he said.
NEXT: Best practices
Treating skin of color acne patients
Controlling inflammation associated with acne is paramount in skin of color patients, given the higher risk for long lasting sequelae, such as postinflammatory hyperpigmentation and, in severe cases involving the trunk, keloids, Dr. Alexis said.
“This can be achieved by careful selection of well-tolerated and effective agents that have antiinflammatory effects relevant to acne. These include topical retinoids [especially adapalene], topical dapsone, and, indirectly, topical benzoyl peroxide, which inhibits P. acnes--an important driver of inflammation in acne,” he said. “It also includes oral tetracyclines [doxycycline and minocycline, in particular].”
READ: Alternative treatment options for acne
Best practices
It might be intuitive for dermatologists to undertreat skin of color acne patients because of the risks of hyperpigmentation and scarring. But that’s not the right approach. In fact, Dr. Alexis said, undertreating skin of color patients with acne could lead to more severe postinflammatory hyperpigmentation. And, in the case of moderate-to-severe truncal acne, undertreatment could increase the risk of hypertrophic or keloid scarring.
READ: Acne ingredients to embrace or avoid
“Carefully select efficacious, but well tolerated topical regimens such that irritation is avoided [since this can induce pigment alterations]. Examples of well tolerated agents are those with well formulated vehicles, such as aqueous gels and creams [as opposed to ethanolic gels which are more drying and potentially irritating],” he said. “Starting retinoids at a lower concentration, then working upward over time is a good strategy to ensure tolerability. Using benzoyl peroxide at concentrations of 2.5- 5% is preferred over higher concentrations. Micronized or micro-dispersed formulations are also better tolerated.”
More on Acne
Gold microparticles zap sebaceous follicles
Acne-fighting collection aims to clear problem skin
NEXT: References
Disclosure: Dr. Alexis is an investigator for Allergan and a consultant or advisory board member with Allergan, Bayer, Galderma and Valeant.
References:
1. Alexis AF. Acne vulgaris in skin of color: understanding nuances and optimizing treatment outcomes. J Drugs Dermatol. 2014 Jun;13(6):s61-5.
2. Callender VD, Alexis AF, Daniels SR, Kawata AK, Burk CT, Wilcox TK, Taylor SC. Racial differences in clinical characteristics, perceptions and behaviors, and psychosocial impact of adult female acne. J Clin Aesthet Dermatol. 2014 Jul;7(7):19-31.
3. Alexis AF, Johnson LA, Kerrouche N, Callender VD. A subgroup analysis to evaluate the efficacy and safety of adapalene-benzoyl peroxide topical gel in black subjects with moderate acne. J Drugs Dermatol. 2014 Feb;13(2):170-4.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.












