- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Adjunct molecular tests aid melanoma diagnosis
Author(s):
Molecular assays have been proven to assist in the diagnosis and prognosis of malignant melanoma. One expert expects that these molecular assays will play a central role in the future treatment and management of malignant melanoma.
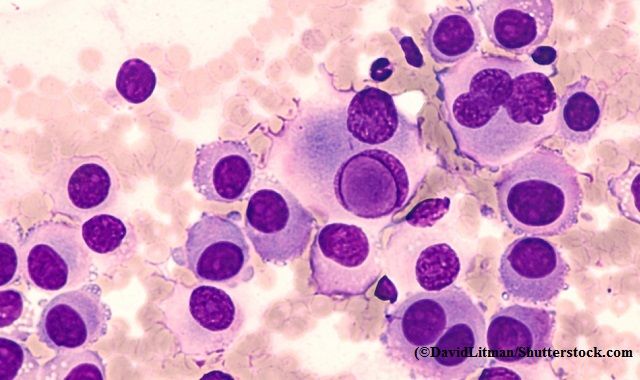
“We have different molecular tests for different purposes depending on how far along in the process we are when assessing the melanoma,” says Pedram Gerami, M.D. (DavidLitman/Shutterstock.com)
The increasing incidence of malignant melanoma has led to continued research on innovative diagnostic and prognostic techniques to help clinicians optimize the treatment and management of the disease. As a result, a variety of molecular assays have been developed to help clinicians better treat and manage melanoma patients. One expert expects that these molecular assays will play a central role in the future treatment and management of malignant melanoma.
“We have different molecular tests for different purposes depending on how far along in the process we are when assessing the melanoma,” says Pedram Gerami, M.D., professor of dermatology and pathology, director of the Skin Cancer Institute of Northwestern Medicine (SCIN-med), director of the Melanoma Program of SCIN-med, Northwestern University Department of Dermatology and the Lurie Cancer Center, Chicago. “Those tests, aimed at accurately diagnosing suspicious pigmented lesions, are designed to differentiate between benign versus malignant, while others look at factors related to the prognosis of the tumor, impacting further treatment decisions and outcomes.”
PRE-BIOPSY DIAGNOSTIC AID
One molecular assay developed by DermTech that assists in diagnosis works by non-invasively collecting skin samples with adhesive patches. An adhesive patch is applied to the surface of the lesion in question. The top skin cells are then analyzed with RT-PCR for gene expression of melanoma associated markers, including LINC and PRAME. The test result is objective and is either positive or negative for gene expression. A positive result generally leads to a biopsy and negative result generally leads to monitoring.
The technique has also been shown to be highly accurate with sensitivity of 91% and specificity of 69%, and a 99% negative predictive value. One limitation of the test is that it can only be implemented in lesions larger than 5 mm and cannot be used on the palms, soles, or mucous membranes.
According to Dr. Gerami, this technique can be useful for diagnostically challenging lesions and could be considered as a noninvasive type of alternative to a traditional surgical biopsy in select cases.
AUGMENTING BIOPSY
In case a biopsy has already been performed, other molecular tests that can assist clinicians more accurately diagnose suspicious pigmented lesions that may still be ambiguous histologically include those that look at chromosomal copy number changes. Fluorescent in situ Hybridizatio (FSH) and Comparative Genomic Hybridization (CGH) are two molecular assay techniques that have been studied very extensively for this purpose, Dr. Gerami says. They can be very useful to help predict which indeterminate or borderline lesion may likely have tendency to behave aggressively, he adds.
“Tumors that have clonal segmental or fragments of the chromosome that have extra copies or losses in them is a pattern that is suggestive of melanoma. Both the FSH and CGH techniques are two alternative methods to analyze tumors and see if they have different dosage of or different levels of certain genes, either losses or gains of certain cancer controlling genes that would favor melanoma," Dr. Gerami says.
Other techniques also useful in morphologically ambiguous cases under a microscope include the mRNA expression profiling test (Castle Biosciences) and the Myriad Genetics myPath test (Myriad Genetics), he says.
Similar to the adhesive tape stripping test method, the mRNA expression profiling test also uses PCR and looks for which genes are turned on and which ones are turned off. The Myriad Genetics myPath test looks at the expression of a total of 23 different genes and which of those genes are turned on or off by the same technique.
“Interestingly, PRAME is also one of those genes analyzed in this test, similar to the target in the adhesive tape stripping test. As such, PRAME appears to be an important gene whether it is turned on or off and can be informative as to whether a lesion is malignant or not,” Dr. Gerami says.
The technique has also been proven in extensive studies to differentiate between benign and malignant lesions with 90% accuracy, Dr. Gerami says. The shortcoming in the testing for this particular technique however is that there has not been any solid validated information for lesions that are completely ambiguous to pathologists.
PROGNOSTIC AIDS
Once melanoma diagnosis has been established, an innovative molecular assay that can be used to help in the prognosis is the Decision-Dx melanoma gene expression profiling test (Castle Biosciences). Prognosis requires traditional staging and includes looking at parameters like Breslow depth and mitotic index to help clinicians discern whether a melanoma is early stage or more advanced in development. Decision-Dx test is a way to use molecular diagnostics to prognosticate or stage the disease as aggressive or not aggressive. Similar to other techniques as far as mRNA expression profiling, the assay of 31 genes also looks at which genes are turned on or off.
“The Decision-Dx melanoma gene expression profiling test has been shown to identify between 75- and 80% of those patients who basically are going to have metastatic disease, but otherwise by their other tests look like they may not have very aggressive stage disease. It is very good at identifying through molecular means looking at the tumor which genes are turned on and off, which of these melanomas is likely to be aggressive even if their traditional staging parameters don’t show it to be,” Dr. Gerami says.
A theoretical limitation of this molecular assay is that, although it has been studied quite extensively with different groups, achieving reproducible results, most of the larger studies were retrospective with only a few small studies with prospective data.
Dr. Gerami says it is important for dermatologists and physicians to embrace these new techniques and not shy away from them perhaps out of concern that such advances could replace them. And, he says, not to worry over becoming proficient with these new methods.
“These molecular assays have already become popular usage in other types of tumors like breast cancer. I believe that it is imperative that dermatologists step up and try to be active leaders in this niche before other specialties in this quickly evolving field,” Dr. Gerami said. Â
Disclosures:
Dr. Gerami reports having consulted with Castle Biosciences, Inc – C(H); DermTech – C(H); Myriad Genetics Inc – C(H)
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.















