- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Black and Asian Patients With Apocrine Adenocarcinoma Demonstrate Significant Risk of Developing Secondary Primary Malignancies
Author(s):
Researchers explored the risk of SPM in patients of different races with the rare type of tumor of the skin.
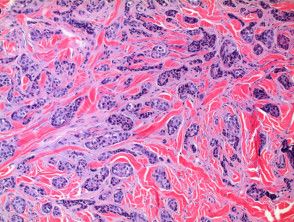
Apocrine adenocarcinomas (AA) are rare adnexal tumors of the skin commonly located in regions with high sweat gland density. They can often be aggressive in nature, with metastatic dissemination, often with lymph node invasion, occurring in approximately 30% of patients.1
A study, titled, "Assessment of Secondary Primary Malignancies in Apocrine Adenocarcinoma by Racial Group," was included in a poster, authored by Kripa Ahuja of Eastern Virginia Medical School, at the 2024 Skin of Color Society Scientific Symposium ahead of the American Academy of Dermatology Annual Meeting in San Diego, California, in March.2
The study and poster explored the risk of secondary primary malignancies (SPMs) in patients of different racial demographics, seeking to compare risk and rates of SPMs in patients with skin of color versus White patients. According to Ahuja, data assessing the risk of SPMs in patients with AA and skin of color are limited, as reported cases of AA are most often attributed to White patients.
Background and Methods
The study involved a search of the Surveillance, Epidemiological, and End Result database. Research involved determining the risk for SPM among patients who had been diagnosed with AA and had survived at least 2 months since the time of diagnosis.
Using Observed: Expected ratios, the study's investigator was able to calculate risk of SPMs among survivors of AA versus individuals of the general population. Statistical significance was established as a p-value of <0.05 with 95% Confidence Intervals.
Findings
In total, the research amassed 3,224 cases of patients with AA of varying races, including White, Black, Asian, Hispanic, American Indian, and patients of other unspecified race populations.
The vast majority of patients were White (n=2,194; or 68%). Fewer cases were attributed to patients of color, with 11% (n=368) being Black, 10% (n=335) being Asian, and 9% (n=286) being Hispanic. Approximately 1% of patients were of unknown race populations (n=28), and less than 1% of patients (n=13) were classified as American Indian.
Compared to White patients, individuals who were Black or Asian exhibited higher risks of developing SPMs, regardless of site/location of AA. White patients demonstrated an Observed: Expected ratio of 1.22 with a 95% Confidence Interval of 1.06-1.39. Black patients demonstrated an Observed: Expected ratio of 1.78 with a 95% Confidence Interval of 1.31-2.37, while Asian patients exhibited an Observed: Expected ratio of 1.22 with a 95% Confidence Interval of 1.07-2.24.
Both Black and Asian patients were the only patients to demonstrate a statistically significant risk of developing SPMs as a result of AA.
Alone, Black patients were the only racial demographic with a significant risk of developing an SPM of the lungs with an Observed: Expected ratio of 2.31 and a 95% Confidence Interval of 1.05-4.38.
Asian patients were among the only group of patients to demonstrate a statistically significant risk of developing an SPM of the tongue with an Observed: Expected ratio of 19.97 and a 95% Confidence Interval of 2.42-72.13.
Conclusions
A limitation of the study, as noted by the study's researcher, is the potential for time length bias.
"Though fewer patients of color develop AA, they have higher rates of developing SPMs," according to Ahuja. "Each race is prone to develop different SPMs."
Moving forward, Ahuja notes that cancer surveillance is warranted in survivors of AA, with particular attention paid to the characteristic and variable of race.
References
- Collette F, Hamoir M, Van Eeckhout P, et al. Metastatic cutaneous apocrine adenocarcinoma successfully treated with systemic anti-androgen therapy-A case report. Clin Case Rep. 2020;8(12):3472-3478. October 30, 2020. doi:10.1002/ccr3.3434
- Ahuja K. Assessment of secondary primary malignancies in apocrine adenocarcinoma by racial group. Poster presented at: 20th Annual Skin of Color Society Scientific Symposium; March 7, 2024; San Diego, California.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.