- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
GEP testing promising in melanoma
Author(s):
GEP testing could improve staging accuracy and help streamline disease management, but more research is needed to determine if a high-risk GEP classification is associated with improved response to newer systemic therapies.
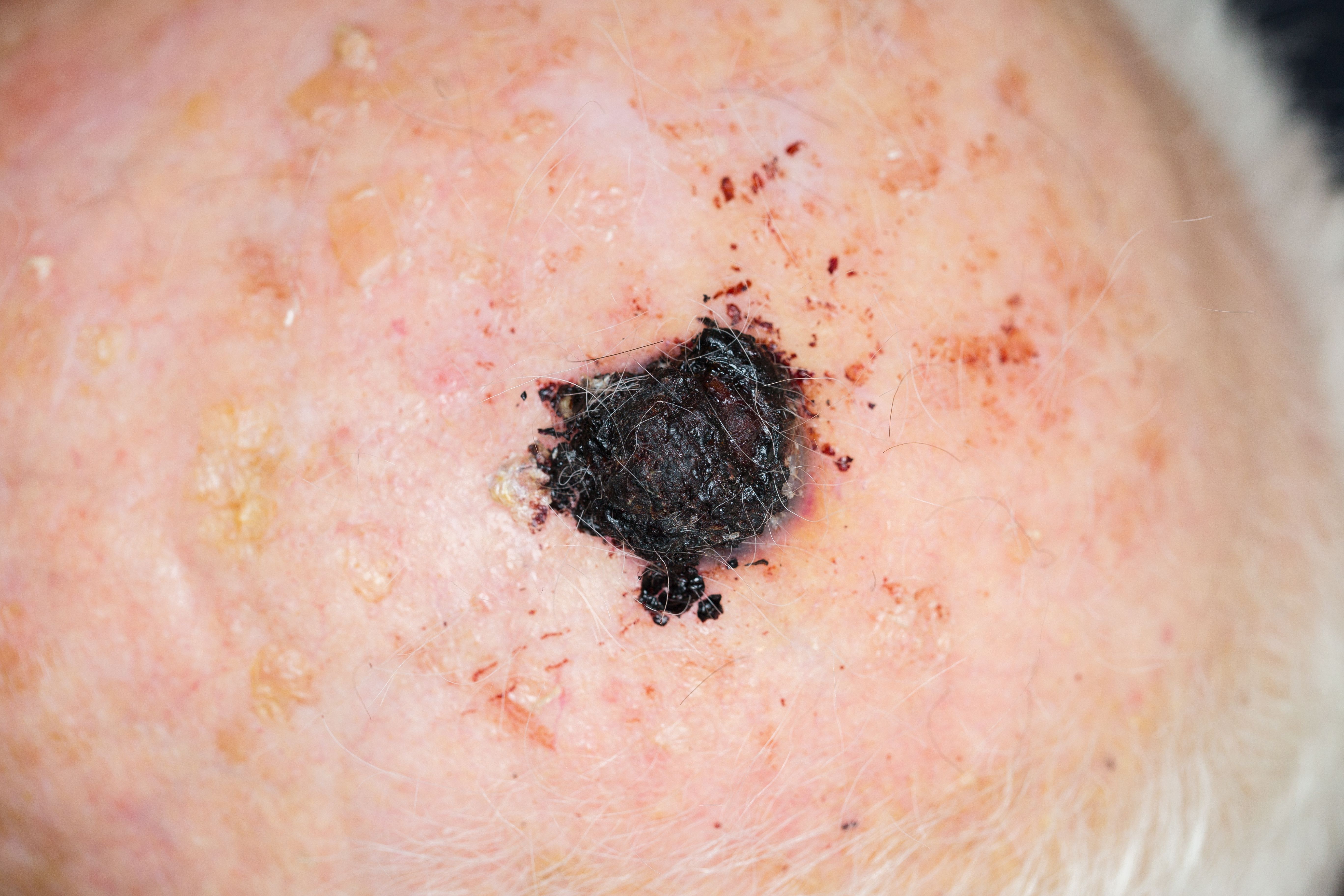
“Patients identified by GEP testing to be at increased risk of disease recurrence and metastasis may benefit from enhanced surveillance, including imaging and physical examination, as well as newer adjuvant therapies,” says Dr. Grossman. (lavizzara - stock.adobe.com)
Dr. Grossman
Gene expression profiling (GEP) testing has the potential to improve prediction of the biological behavior of melanocytic lesions by objectively defining “high-risk” on a molecular level, according to Doug Grossman, M.D., Ph.D., who presented “Update on molecular diagnostic and prognostic tests for melanoma” during the Advances in Melanoma course, Thursday, July 25 at the American Academy of Dermatology’s (AAD’s) 2019 Summer Meeting in New York City.
Molecular tests based on gene expression profiling of cutaneous melanoma are highly sensitive and commercially available. They include the diagnostic tests 23-GEP MyPath Melanoma (Myriad) and 2-GEP Pigmented Lesion Assay (DermTech) and prognostic test 31-GEP Decision-Dx Melanoma (Castle Biosciences), according to Dr. Grossman, professor of Dermatology and Oncological Sciences and investigator at the Huntsman Cancer Institute, University of Utah.
“Patients identified by GEP testing to be at increased risk of disease recurrence and metastasis may benefit from enhanced surveillance, including imaging and physical examination, as well as newer adjuvant therapies,” Dr. Grossman tells Dermatology Times. “Validated GEP testing could improve staging accuracy and help to streamline management. For instance, GEP test results could inform which patients might benefit from more or less aggressive treatment, such as wider or narrower excision margins for their primary cutaneous melanoma; undergoing or avoiding a sentinel lymph node biopsy procedure; and receiving or foregoing surveillance imaging or systemic adjuvant therapy.”
Despite the potential of the testing, gaps in research remain.
Current melanoma guidelines from the AAD and the National Comprehensive Cancer Network recommend further study of GEP tests before clinicians incorporate them into clinical practice for cutaneous melanoma. Nevertheless, clinicians’ use of the testing for diagnosis and prognosis is becoming more prevalent, according to Dr. Grossman.
“… it is not currently known whether a high-risk GEP classification or pre-symptomatic detection of distant metastasis, through surveillance imaging, is associated with improved response to newer systemic therapies,” he says. “We will need high-quality clinical trials to determine best use of GEP testing for our patients.”
Disclosures:
Dr. Grossman has no conflicts with companies involved in GEP testing. He serves on the advisory board of Orlucent.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.














