- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
Lab, clinical background key in pediatric dermatopathology
Even with relatively recent advances such as immunohistochemical staining and molecular analysis, experts say, pediatric dermatopathology relies heavily on clinical correlation.
Top pediatric dermatopathologists wield advances such as immunohistochemical staining and genetic testing in the context of clinical insight.
Critical combination
Unfortunately, says Jan Izakovic, M.D., not all dermatopathologists regularly deal with pediatric dermatopathology. And among those who do, he says, even fewer have both laboratory and clinical backgrounds. Dr. Izakovic is a voluntary associate professor of dermatology at the University of Miami and a Basel, Switzerland-based dermatologist who consults in pediatric dermatology at the University Children's Hospital of Basel.
Recommended: Biopsy process helps pathologists determine accurate diagnosis
"You need this combination-people who see pediatric patients clinically, and have a second specialization in evaluating specimens under the microscope." When doing so, "They have the clinical picture of the condition in mind. A pure pathologist wouldn't necessarily."
That's important, says Dr. Izakovic, because even under the microscope, some dermatologic conditions – particularly inflammatory ones such as psoriasis and eczema-can look similar, and dermatopathologists must discriminate based on minute details.
Therefore, he says, dermatopathologists like to request digital clinical images, which can be particularly helpful in distinguishing between two potential diagnoses. The correlation between the clinical image and what he sees on the cellular level helps him to make the final diagnosis.
Also read: Dermatopathology sits in healthcare reform crosshairs
Dallas-based Fred Ghali, M.D., adds that for pediatric dermatologists such as himself, "Establishing clinical-pathological correlation is key to the proper diagnosis. In some cases, it may be very difficult to narrow my clinical differential diagnosis until I have the pathology to direct me to a certain category of disease. Connective tissue diseases such as lupus erythematosus, morphea and dermatomyositis, as well as rare disorders of the fat such as panniculitis, are examples of conditions a dermatopathologist can help diagnose when the clinician is considering a whole host of possible skin disorders."
Read: New medical therapies result in symptoms of various skin conditions
Malignancies, albeit rare in the pediatric population, can sometimes present in infancy, Dr. Ghali says, adding that establishing a predominant cell type histologically helps to make the diagnosis as early as possible, and furthermore, to assist the clinician in choosing the optimal therapy.
NEXT: Melanoma mimics

A congenital growth located on the scalp of an infant was consistent with leukemia cutis on pathology.
Melanoma mimics
Because cancer occurs much less commonly in children than adults, says Clay J. Cockerell, M.D., "If we see an atypical melanocytic lesion in a child, we're very loath to diagnose melanoma" unless the sample shows virtually every textbook feature. He is a Dallas-based dermatologist and dermatopathologist who owns Cockerell Dermatopathology Laboratory.
Read: Melanoma detection involves more than using ABCDs
Occasionally, in a child or baby, "We'll get a congenital nevus that has a large proliferating nodule in its center. That can simulate melanoma, but it's not." Making the distinction generally requires a good dermatopathologist who knows that with such nevi, "You can get a large number of these cells that look more primitive. Even though it's a nodular proliferation, they tend to have relatively few mitotic figures, and the cytologic atypia is not as great as one would see in malignant melanoma."
Beyond basic histology, says Dr. Izakovic, dermatopathologic techniques used for pediatric skin conditions – benign or malignant – increasingly include immunohistochemical staining and molecular genetic analysis. The biggest breakthrough, says Dr. Ghali, has come with molecular analysis of chromosomal aberrations, using either comparative genomic hybridization (CGH), or fluorescent in-situ hybridization (FISH).1 With this additional analysis, he says, "We are able to better differentiate an atypical Spitz nevus from melanoma. Nothing is 100%, but molecular analysis gives us more evidence to support whether something is benign or malignant."
NEXT: Melanoma mimics

Histopathology of this vascular lesion located on the right flank of a neonate proved to be a tufted angioma. GLUT-1 staining was negative in this case.
In a recent case treated by Dr. Cockerell, a young child had a very atypical-looking lesion that FISH and the MyPath test (Myriad Genetics) confirmed was malignant melanoma, which ultimately spread to several lymph nodes. Nevertheless, "The child did not develop widespread disease. We're beginning to see some cases of these atypical Spitzoid lesions in children,"2 who tend to fare better than adults with similar lesions, for reasons that remain unclear.
In the past, says Dr. Cockerell, dermatopathologists would largely shrug off many atypical benign Spitz nevi as being "Spitz variants with different histologic findings." Recently, he says, genetic testing has revealed that these variants may have specific mutations or anaplastic lymphoma receptor tyrosine kinase (ALK) fusions. "The ALK-fusion lesions have spindle-cell melanocytes with plexiform growth pattern. Clinically, they are polyploid and amelanotic," he notes. Fortunately, "They still behave in a benign fashion."
Recommended: Screening labs, complacency, and the ABCDEs of pediatric melanoma
With Spitz nevi, Dr. Izakovic says, distinguishing between benign and malignant lesions may prove difficult. Spitzoid melanoma often appears similar to a Spitz nevus, he explains. "While the majority of the lesion appears benign, in some area of the specimen, there are clusters of more atypical, malignant-looking cells. This may cause you to think, 'It's starting to transform into something malignant.' Looking just at cell morphology, it might look like melanoma." In combination with the more typical Spitzoid portion, however, "It's not a straightforward melanoma like you would typically see in an adult. It's a pediatric type of melanoma."
With diagnostic dilemmas such as "STUMP (Spitzoid tumor of uncertain malignant potential)" lesions, many patients and physicians alike seek second opinions from both the pediatric dermatologist and the dermatopathologist, says Dr. Ghali. Consequently, he says, collaboration between the 2 sub-specialties, as in the case of Drs. Cockerell and Ghali, improves the diagnostic evaluation in these most challenging cases.
Also read: Opportunities, challenges with new treatments for advanced cancer
Histochemical stains such as p16 staining can be of benefit, says Dr. Ghali. "For example, positive p16 staining would tend to favor more of a benign process, whereas loss of staining would favor melanoma," he says. Other immunohistochemical stains that can be used to help discriminate atypical Sptiz nevi or melanoma include expression of p53 stain and Ki-67.
NEXT: knowing when it's benign
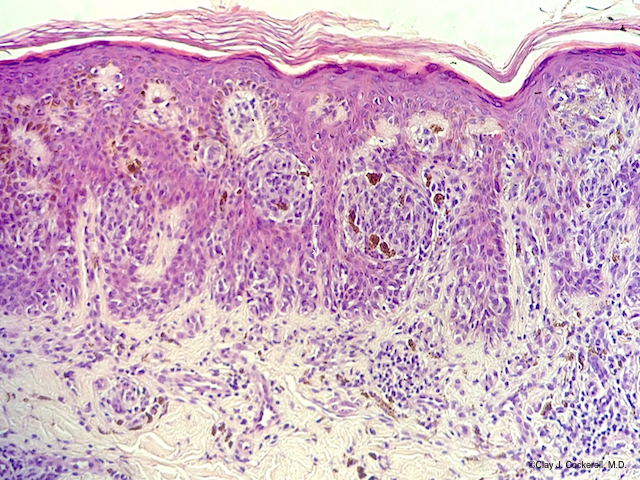
Typical histologic image of a Spitz nevus, demonstrating nests of epithelioid melanocytes and pink globules known as Kamino bodies.
Knowing when it’s benign
Pediatric lesions also may demonstrate basal cell carcinoma (BCC)-like features on microscopic examination, says Dr. Cockerell. "The vast majority are benign lesions like trichoepitheliomas. Thus, it's important for anybody evaluating a pediatric case to be aware of these entities that can simulate cancer but really are not."
Read: Sonidegib offers new option for basal cell cancer
Dr. Cockerell notes that children can, not uncommonly, develop another benign congenital nevus, nevus sebaceus. "These lesions often develop benign follicular trichoblastomas within them. For years we thought they were BCCs arising in the setting of a nevus sebaceus, but we now know that most of these really are not BCC-they’re actually follicular hamartomas that look like BCC microscopically." Like BCC, "They have a very slow, indolent biologic behavior."
When considering vascular malformations and hemangiomas, says Dr. Cockerell, "We have the ability to look for glucose transporter-1 (GLUT-1) expression. Dr. Ghali added, "GLU T-1 is positive in hemangiomas of infancy (HOI), most of which regress, but negative in vascular malformations which do not involute and grow larger as the child grows." GLUT-1 is also not expressed in congenital hemangiomas, which have been divided into those which involute rapidly (rapidly involuting congenital hemangioma, RICH), those which do not involute (non-involuting congenital hemangioma, NICH) and those which only partially involute (partially involuting congenital hemangiomas, PICH). Other vascular lesions that fail to express GLUT-1 are tufted hemangiomas and Kaposiform hemangioendotheliomas.
Read: The role of the dermatologist in diagnosing, managing advanced basal cell carcinoma
However, Dr. Cockerell says, "Just because it's GLUT-1 positive doesn't necessarily mean it's going to regress completely and leave normal-appearing skin."
Because the number of biopsies performed in children is lower than in adults, says Dr. Cockerell, it's important to work with a dermatopathologist who has experience in evaluating pediatric skin biopsies. For the dermatopathologist, he says, "It's rewarding to work with an excellent pediatric dermatologist like Dr. Ghali to solve these sometimes difficult riddles in kids. You don't want to overcall something and cause a panic in the family, but you don't want to miss something dangerous like a serious infection or rare tumor in a child. Having good clinical correlation is vital."
Disclosures: Dr. Cockerell is a speaker and consultant for Myriad Genetics. Drs. Izakovic and Ghali report no relevant financial interests.
References:
1. Tom W, Hsu JW, Eichenfield LF, Friedlander SF. Pediatric STUMP lesions: evaluation and management of difficult atypical Spitzoid lesions in children. J Am Acad Dermatol. 2011;64:559-72.
2. Hung T, Piris A, Lobo A, et al. Sentinel lymph node metastasis is not predictive of poor outcome in patients with problematic spitzoid melanocytic tumors. Hum Pathol. 2013;44(1):87-94.





