- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Lichen Sclerosus Present in 82% of Penile Melanomas
Author(s):
While the linkage between squamous cell cancers and genital lichen sclerosus has been well-established, fewer studies have examined the associations between penile melanomas in males.
In a recent study1 published in Skin Health and Disease, researchers found that genital lichen sclerosus (GLSc) was present in 82% of penile melanoma (PeMM) cases.
David A. Litman/AdobeStock
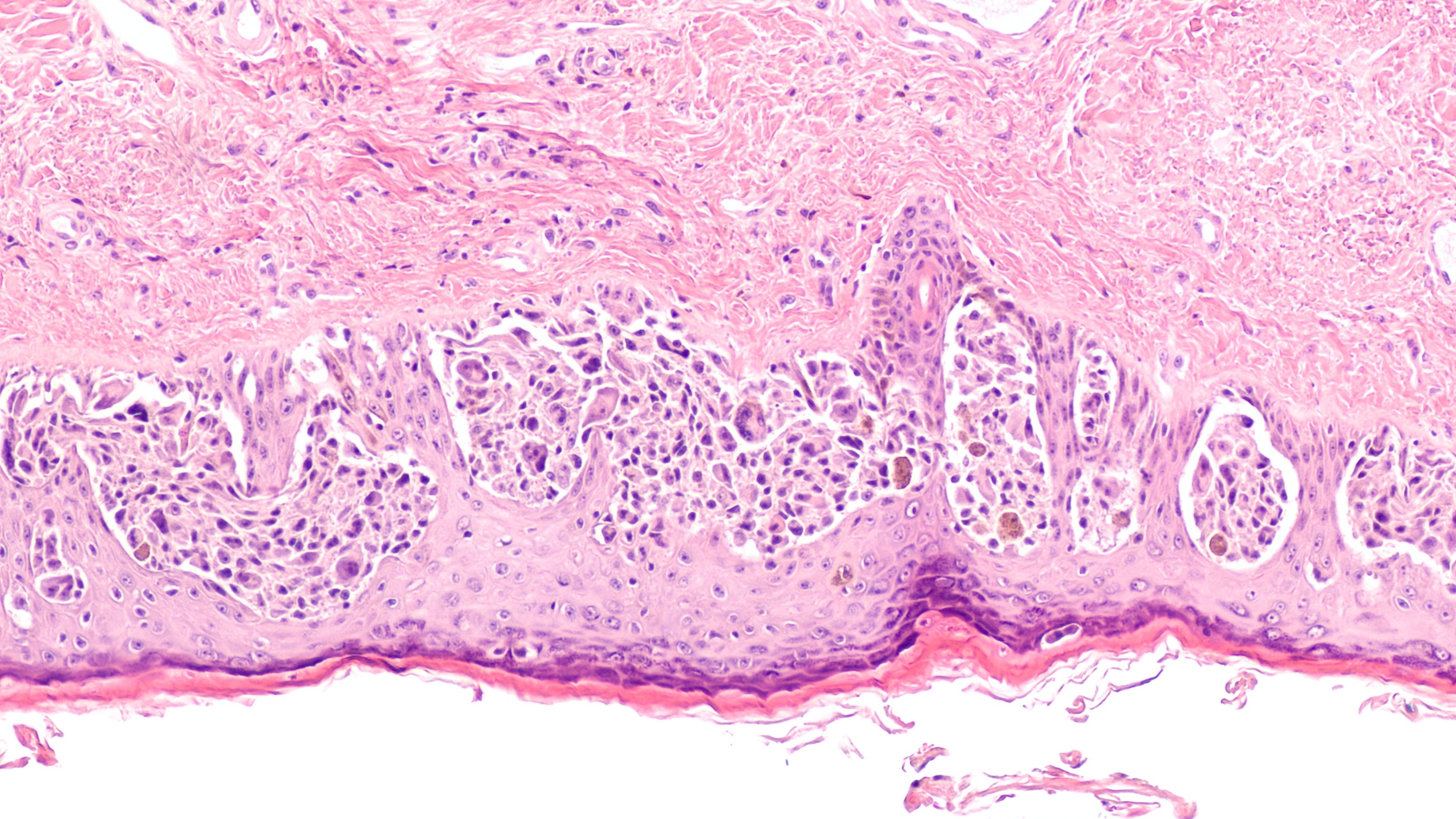
According to researchers Dear et al, the associations between squamous cell cancers and GLSc are well-established, as well as several reported cases of vulvar melanoma (MM) present in the literature. However, there have not been any studies linking the relationship between GLSc and genital melanoma in the male population; in such reports in the literature, these have been limited exclusively to case studies.
In order to explore the relationship between male GLSc and PeMM, researchers reviewed all relevant cases from a tertiary urology and male genital dermatology service. The retrospective analysis included patients with a PeMM diagnosis and available histopathology to review. All patients had been seen between the years 2011 and 2022.
Clinical records and photographs were first reviewed by a team of 2 dermatologists while 2 histopathologists conducted independent reviews of patient histopathology and features of GLSc.
Eleven patients with PeMM were identified, and researchers collected clinical and demographic information relevant to the study, including age at diagnosis, ethnicity, features of GLSc, and melanoma subtype, stage, and mutation, when applicable.
In 9 of the 11 cases, or 82% of patients, GLSc was present in histopathology. These patients were found to have clinical features of male GLSc.
Prior to this study, there have only been 3 documented cases of GLSc and PeMM comorbidity.
“In addition to being under-recognised clinically, GLSc in the context of MM might also be under-recognised histologically,” according to Dear et al. “The histopathological confirmation of the presence of LSc in nine out of eleven men with PeMM seen at our tertiary centre does not prove a causative relationship between GLSc and PeMM but is suggestive. We theorise that this is related to chronic melanocytic distress created by LSc. Our findings have implications for the prevention, early diagnosis, management, and follow-up of MGLSc.”
Reference
- Dear K,Kravvas G, Sim S, et al. Primary penilemelanoma and genital lichensclerosus. Skin Health and Disease. Published online 2023. doi:10.1002/ski2.274
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.















