- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Oncology Pharmacists Are Crucial in Skin Cancer Management
Author(s):
From explaining how medications work and should be taken to reviewing potential adverse effects and financial details, pharmacists are crucial resources for patients undergoing treatment for skin cancer.
Photo courtesy of the CDC Public Health Image Library

Skin cancer is the most diagnosed malignancy in the United States today, with the American Academy of Dermatology estimating that 20% of Americans will develop skin cancer in their lifetime, and approximately 9500 individuals in the United States are diagnosed with skin cancer every day.1 Pharmacists play a vital role in educating patients on how to protect the skin from the sun, which limits risk factors of skin cancer, according to the California Pharmacists Association.
“Counseling patients about safe sun exposure enhances pharmacists’ professional satisfaction,” a spokesperson for the association said. “To provide effective patient education, pharmacists [must] keep abreast of new product developments and understand the detrimental effects of sun exposure.”
Pharmacists also play a big role during the treatment phase by explaining to patients how various medications work, reinforcing how they should best be taken, reviewing any potential adverse effects, and going over insurance and financial details.
Chelsey Lindner, PharmD, clinical pharmacist at Shields Health Solutions in Stoughton, Massachusetts, is a board-certified oncology pharmacist who has worked with patients with skin cancer from within a health-system specialty pharmacy for more than 6 years. “Prior to the COVID-19 pandemic, I worked onsite with an outpatient integrated care team, meeting with patients face-to-face who were starting oral targeted agents, such as BRAF/MEK inhibitors for melanoma and hedgehog pathway inhibitors for the treatment of advanced basal cell carcinoma,” she said. “I provided comprehensive education on the safe and effective use of these medications and assisted with [adverse] effect management, adherence, and other monitoring while on therapy.”
Following the pandemic, Lindner has shifted to a remote work setting and now provides these same services via telephone follow-up and primarily communicates with the outpatient care team electronically to coordinate care. One of the biggest challenges of care, Lindner noted, is prolonged tolerability of available therapeutic modalities.
“Many patients abandon a treatment strategy altogether due to development of toxicity, so even if the drug is effectively treating their cancer, they can’t tolerate it [and] we have to move to the next line of therapy,” she said. “[Although] immune checkpoint inhibitors [ICIs] and targeted therapies are the mainstays of treatment for advanced melanomas, 40% to 65% of patients have primary resistance to ICIs.”
Improving the Future
The pharmaceutical industry is looking toward the future by investing in research and in the development of new treatments and diagnostic tools for skin cancers.
“Investigating new drugs and therapeutics, new dosing schedules, and improved risk stratification modalities with aim to improve clinical outcomes, improve tolerability, and better preserve or enhance quality of life [will benefit patients],” Lindner said. “With more convenient dosing forms or schedules and patients on [longer courses of] therapy with greater response rates, it overall enhances ways to personalize treatment for each patient.”
Advances in genetic testing and molecular profiling are helping identify the genetic mutations that drive cancer growth, which in turn can help develop targeted therapies. Additionally, efforts are being made to improve early detection through public education campaigns and the development of new diagnostic tools, such as noninvasive imaging techniques.
“As a pharmacist, my role is to stay up to date with the latest developments in skin cancer treatment,” said Kimberly Shaw, PharmD, a pharmacist in Tempe, Arizona. “[I] work closely with health care providers and patients to provide the best possible care and support.”
Current Treatment Options
“Treatment options for skin cancer depend on the type and stage,” said Kimberly Shaw, PharmD, a pharmacist in Tempe, Arizona. “Surgery, radiation, and chemotherapy are commonly used treatments. Topical treatments such as creams or gels may also be effective for less severe cases.”
Melanoma
Immunotherapy has been particularly effective in treating melanoma. The treatment “works by activating the immune system to fight cancer cells,” Shaw said. There are several immunotherapy drugs available to treat melanoma. Targeted therapies have proven effective in treating melanoma. Research is ongoing to determine its effectiveness in other types of skin cancer.
The primary treatment modality for cutaneous melanoma depends on the extent of the disease; treatment choices can be guided by molecular profiling of the tumor. The goal for early-stage disease “is to remove the tumor and prevent recurrence,” said Chelsey Lindner, PharmD, clinical pharmacist at Shields Health Solutions in Stoughton, Massachusetts. For patients with more advanced stage 2b or 2c disease, pembrolizumab (Keytruda) is a National Comprehensive Cancer Network Category 1 recommendation, she explained.
Patients with high-risk stage 3 disease or recurrent/stage 4 disease should undergo molecular testing to determine whether they are a candidate for BRAF-directed therapy, to gather information about potential additional genetic targets, and/or to determine their eligibility in clinical trial participation.
For patients with high-risk stage 3 disease and a BRAF V600E-activating mutation, treatment options include adjuvant dabrafenib (Tafinlar) plus trametinib (Mekinist). For patients without that genetic marker, systemic treatment with an adjuvant PD-1 immunotherapy, such as nivolumab (Opdivo) or pembrolizumab, may be offered.
For patients with stage 4 oligometastatic disease, resection, stereotactic ablative therapy, or talimogene laherparepvec intralesional therapy may be considered, followed by systemic therapy. “[For] patients with distant metastasis, systemic therapy is preferred. Palliative resection and/or radiation may be offered for symptomatic extracranial disease,” Lindner said. She also explained that the preferred systemic regimens for metastatic or unresectable disease include combination checkpoint blockade, such as nivolumab/ipilimumab or nivolumab/ relatlimab-rmbw; anti-PD-1 monotherapy, such as pembrolizumab or nivolumab; or combination targeted therapy, such as dabrafenib/trametinib, vemurafenib (Zelboraf)/cobimetinib (Cotellic), or encorafenib (Braftovi)/binimetinib (Mektovi), if a BRAF V600E-activating mutation is present.
Basal Cell Carcinoma
The primary treatment for basal cell carcinoma (BCC) depends on patient risk status and the extent of disease at presentation, Lindner explained. “The ultimate goal is to eliminate the tumor while maximizing preservation of function and physical appearance.”
In cases of superficial BCC, topical therapies such as imiquimod, 5-fluorouracil, photodynamic therapy, or cryotherapy can be considered; however, cure rates may be lower. Primary treatment for localized BCC consists of tumor removal, with a method dependent on tumor location, size, and depth. Radiation may be offered to patients with higher risk factors or for whom tumor removal is not possible.
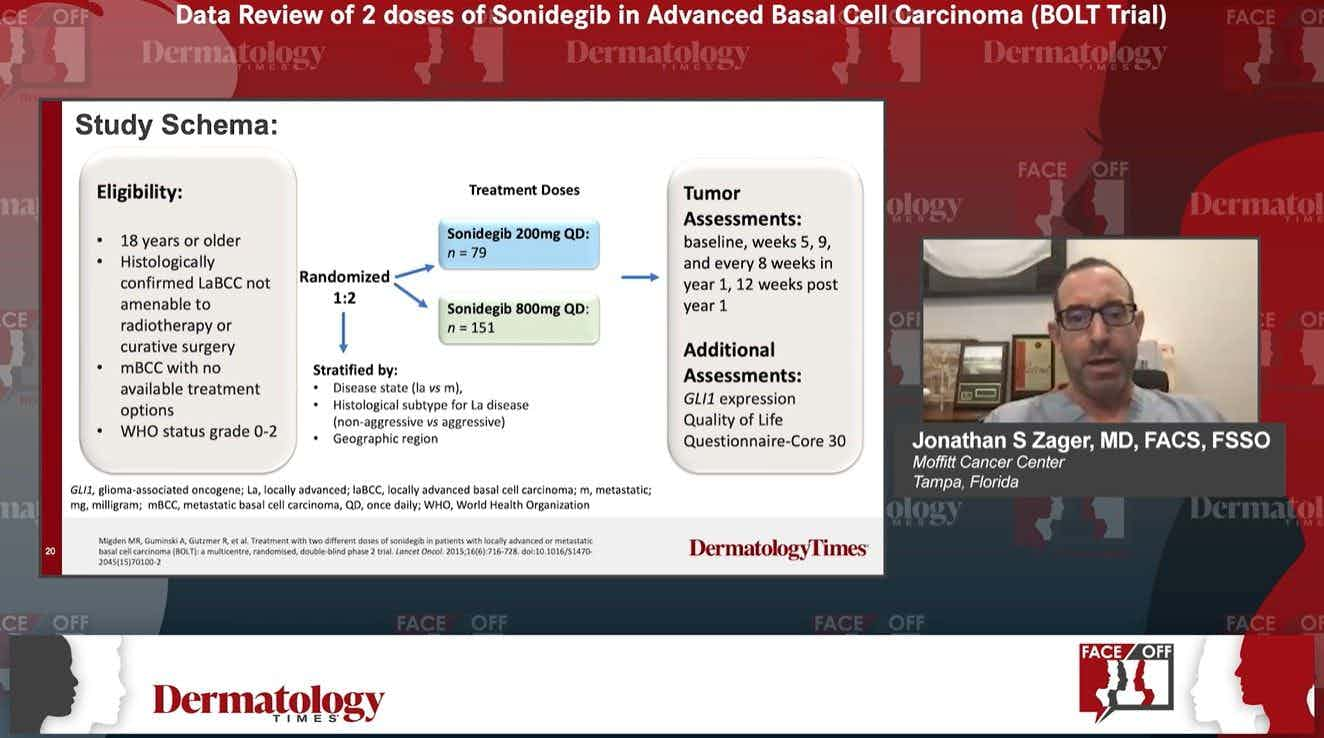
Systemic treatment may be available for patients with localized disease who are not eligible for radiation or surgery, or for patients with more advanced BCC, including regional or distant metastases. Systemic treatment options include hedgehog pathway inhibitors vismodegib (Erivedge) and sonidegib (Odomzo), as well as PD-1 antibody cemiplimab-rwlc (Libtayo).
Squamous Cell Carcinoma
Surgical excision is the gold standard for cutaneous squamous cell carcinoma, Lindner explained. Treatment typically includes photodynamic therapy, laser treatment, cryosurgery, or radiation therapy. Immune checkpoint inhibitors, including cemiplimab-rwlc or pembrolizumab, can be used in locally advanced and metastatic cases.
Melanoma Treatments in the Pipeline
“There are several new drugs in development that target different genetic mutations in melanoma, and [investigators] are exploring the use of combination therapies that use multiple drugs to attack cancer from different angles,” said Kimberly Shaw, PharmD, a pharmacist in Tempe, Arizona.
T-cell targeted and T-cell manipulative therapies are also promising, as melanoma is one of the most immunogenic tumor types. Further investigation of the therapeutic benefit of neoadjuvant therapy (immunotherapy or BRAF/MEK inhibitors) for resectable melanoma is underway.
EVX-01, a personalized therapeutic vaccine that produced long-lasting T-cell responses, was well tolerated in a phase 1/2a clinical trial. Additionally, a phase 2 clinical trial is currently underway, with a mix of pembrolizumab for metastatic melanoma.
LNS8801, an oral G protein-coupled estrogen receptor agonist, gained orphan drug designation for patients with metastatic or unresectable melanoma who have progressed on anti–PD-1/PD-L1 therapy after showing that it stimulated tumor regression immune memory in preclinical models across various tumor types.
Reference
1. Skin cancer. American Academy of Dermatology. Updated April 22, 2022. Accessed March 13, 2023. https://www.aad.org/media/stats-skin-cancer
[This article was originally published by our sister brand, Drug Topics.]
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.