- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Other skin conditions can mimic signs of rosacea
Clinicians need to keep in mind possible differential diagnoses that mimic rosacea when they see patients who exhibit symptoms that appear to suggest the disease, according to the director of the Bikowski Skin Care Center.

Key Points
Sewickley, Pa. - Clinicians need to keep in mind possible differential diagnoses that mimic rosacea when they see patients who exhibit symptoms that appear to suggest the disease, according to the director of the Bikowski Skin Care Center.

"Rosacea classically presents as erythematous papules and pustules with flushing and blushing of the central third of the face," Dr. Bikowski says. "There may be an erythematous background and telangiectasia present."
Might be mites
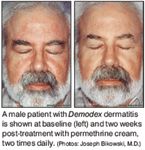
Demodex dermatitis, which Dr. Bikowski says he is seeing with increasing frequency in his clinical practice, is characterized by a diffuse erythema and fine observable and palpable scaling that is present on sites such as the forehead, nose, cheeks and chin. Indeed, the diagnosis may be masked by other skin conditions such as papulopustular rosacea or seborrheic dermatitis.
Both irritant and allergic contact dermatitis, as well as lupus, are other conditions that can resemble rosacea, according to Dr. Bikowski.
"The issue is whether everything that is on the face that is red and scaly is rosacea or not," he says. "Because rosacea and seborrheic dermatitis are very common conditions, they often may occur together. You often see the classic, clinical presentation of rosacea, with the dryness and scaling of seborrheic dermatitis. A number of patients, especially those who don't respond to the usual rosacea and seborrheic dermatitis treatments, have Demodex dermatitis."
The Demodex mite lives in the hair follicles on the face. Rosacea is not believed to be caused by Demodex mites, but some patients have a heightened response to the presence of these mites on the face.
"There is a certain percentage of the population that has an increased reaction to the presence of this mite or the mite products, producing Demodex dermatitis," Dr. Bikowski says.
He stresses that there is no proof that the Demodex mite causes rosacea. "I think the mite produces a separate condition which is recognizable and treatable," he says.
Ruling out mites
To exclude Demodex dermatitis in the differential diagnosis, Dr. Bikowski suggests clinicians opt for topical treatment in the form of permethrin or crotamiton cream, applied twice daily, for two to four weeks.
"If you have a therapeutic trial of each of those products, about a third of the patients will clear (the condition) within two to four weeks with that therapy," Dr. Bikowski says. "If they do not clear, then you know that you have rosacea and/or seborrheic dermatitis."
Dr. Bikowski contrasts the goals of therapy in managing rosacea and/or seborrheic dermatitis compared to the goals of therapy in managing Demodex dermatitis.
"The best you can hope to achieve over the short term or long term if you make a diagnosis of rosacea and/or seborrheic dermatitis is to treat and control," Dr. Bikowski says. "Demodex dermatitis can theoretically be 'cured' in two to four weeks, and patients can stay clear of the condition for months and even years."
While there is no time urgency in treating Demodex dermatitis - the condition will not worsen and become grave - the failure to make a correct diagnosis is a failure to treat the condition in a timely fashion, Dr. Bikowski says.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.











