- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Out of the norm: Purpura annularis telangiectodes of Majocchi uncommon
Author(s):
Making an accurate diagnosis of a given dermatosis can be easy when the clinical symptoms and the patient population are textbook presentations; however, exceptions make the rule.
New York ‖ The appearance of textbook clinical symptoms in dermatologic diseases normally allows the clinician to arrive at a quick and accurate diagnosis. However, clinicians are sometimes taken by surprise when typical clinical symptoms for a given dermatosis appear in patient populations other than classically described, as was the case in two recent clinical cases of purpura annularis telangiectodes of Majocchi.

Nonblanching annular erythematous petechial patches on lower abdomen in patient two.Photo: Kristyna Lee, M.D., M.P.H.
"We recently saw two patients in our clinic who presented with cutaneous lesions typical of purpura annularis telangiectodes of Majocchi. This rather uncommon dermatosis normally appears in adolescents and young adults and is much more common in females.
Case studies
" However, our two patients were both elderly males which is very different from the classic patient population description of this disease," says Kristyna Lee, M.D., M.P.H., department of dermatology, SUNY Downstate Medical Center, Brooklyn, New York.
The first patient was an 83-year-old Caucasian male with no significant past medical history who presented with a one-week history of non-pruritic multiple discrete 3 cm to 5 cm nonblanchable annular and arcuate purpuric and erythematous patches, which were extensively distributed along the bilateral proximal pretibial and posterior calf and ankle regions.
The second patient was a 79-year-old Caucasian male who also had no significant past medical history and presented with a two-month history of very similar cutaneous lesions along the lower abdomen and posterior waistline.
Both patients denied any history of trauma, preceding illness, prodromal symptoms, new medication use or easy bruisability.
Neither patient showed any abnormalities in the laboratory evaluations which included antinuclear antibody (ANA) titer, coagulation factors and complete blood cell count with differential. Both patients lacked constitutional symptoms and appeared healthy, allowing Dr. Lee to rule out coagulation disorders, vasculitis, thrombocytopenic states or purpuras secondary to acute infections.


Nonblanching erythematous and violaceous annular patches and scattered erythematous macules and petechiae on posterior right calf in patient one.Photo: Kristyna Lee, M.D., M.P.H.
Histopathology for both patients revealed a perivascular and interstitial infiltrate of lymphocytes admixed with red blood cells in the papillary dermis. The diagnosis of purpura annularis telangiectodes was made and both patients were subsequently treated with supportive therapy after which all lesions gradually resolved with residual post-inflammatory hyperpigmentation.
"Purpura annularis telangiectodes is an uncommon disease and considered to be especially uncommon in older and male patient populations. Therefore, we were very surprised when two atypical cases presented in our clinic just within a week of each other.
"I think that dermatologists should be made more aware of the possible occurrence of atypical presentations of dermatologic diseases and always keep an eye out for those cases that break the rule. Such cases are not as uncommon as we may suppose and we should always keep this in the back of our minds when diagnosing patients,” Dr. Lee says.
Variants
According to Dr. Lee, at least five variants of pigmented purpuras are described in dermatology including progressive pigmented purpura or Schamberg’s disease, eczematoid-like purpura of Doucas and Kapetanakis (a possible variant of Schamberg’s disease), lichen aureus, pigmented purpuric lichenoid dermatosis of Gougerot and Blum and purpura annularis telangiectodes of Majocchi.
Dr. Lee says that of these five variants, purpura annularis telangiectodes of Majocchi is one of the more rare types of pigmented purpura, whereas Schamberg’s disease is much more commonly seen and is the most common type of pigmented purpura followed by lichen aureus.
Because of the clinical and histologic overlap seen in these pigmented purpuras, it can sometimes prove challenging to distinguish them from each other, especially if they occur in atypical patient populations, confounding a quick diagnosis.
Etiology
The etiology of purpura annularis telangiectodes remains unknown. Because the lesions occur predominantly on the lower extremities and buttocks, the effects of gravity, orthostatic pressures and elevated venous pressures have been postulated as possible etiologies of the disease.
Another theory states that Langerhans-cell mediated injury and immune-complex deposition resulting in capillary leakage may be the cause of the clinical symptoms seen.
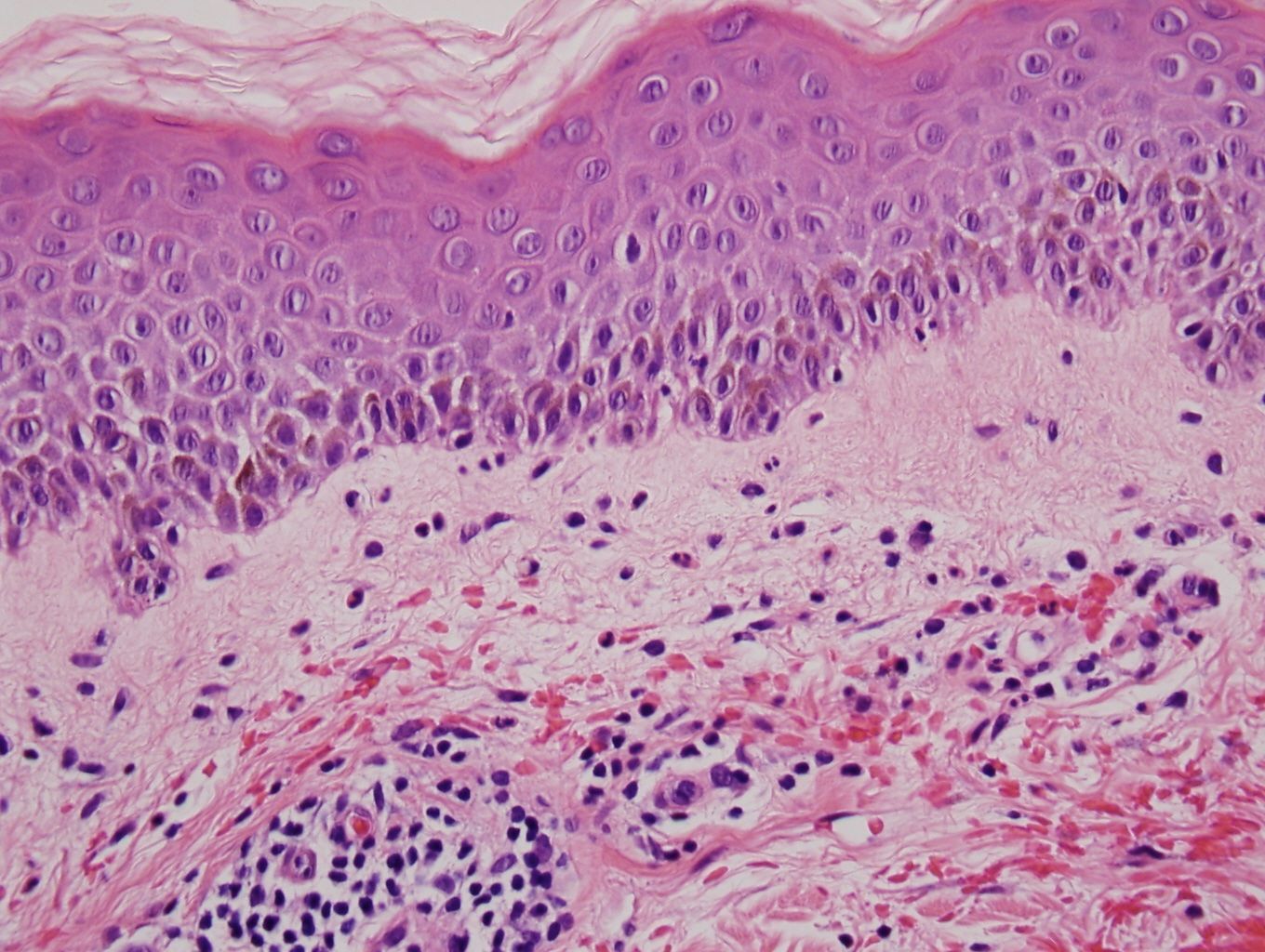
Superficial perivascular and interstitial infiltrate of lymphocytes admixed with red blood cells in the papillary dermis.Photo: Kristyna Lee, M.D., M.P.H.
"Whatever the cause, clinicians should be prepared to expect the unexpected when diagnosing their patients as these two classic clinical presentations occurred in atypical patient populations, underscoring the importance of a heightened awareness dermatologists should have when considering the correct diagnosis in their dermatologic patients," Dr. Lee says. DT
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.













