- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Panniculitis: A multifaceted malady
Author(s):
The various types of this multi-etiologic disease can be categorized as septal, lobular or a combination of septal and lobular panniculitis.
Leslie Robinson-Bostom, M.D., associate professor of the department of dermatology and director of the division of dermatopathology at Brown Medical School, Providence, R.I., discusses panniculitis and reviews the new developments of this subcutaneous inflammation.
Panniculitis particulars
"These nodules are usually but not always tender, can sometimes drain an oily discharge and can sometimes even suppurate. The overlying skin above the nodules may be thickened and indurated on palpation, with or without hyperpigmentation. After the inflammation subsides, a depression in the skin (lipodystrophy) may be left behind, which can be either temporary or permanent. This subcutaneous inflammation can only be diagnosed with a biopsy, preferably an incisional wedge biopsy taken from a fully developed lesion. Once the lesion is identified and a definitive diagnosis can be made, the physician must then begin his search for the cause, of which many are possible," Dr. Robinson-Bostom tells Dermatology Times.
Breaking it down
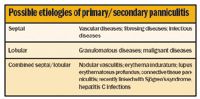
Panniculitis is either primary or secondary.
While primary panniculitis may be traced to a number of specific maladies, secondary panniculitis occurs as a sequela to a multitude of disease states.
Regardless, Dr. Robinson-Bostom explains that although the classification of panniculitis can be somewhat complicated, basically the various types of this multi-etiologic disease can be categorized as septal, lobular or a combination of septal and lobular panniculitis.
The most common cause of primary septal panniculitis is erythema nodosum. The clinical and microscopic features causing this disease are well known to the experienced dermatologist.
The most common etiologic agents in erythema nodosum include infections (e.g. group A beta haemolytic Strep, deep fungal and viral), drugs (e.g. oral contraceptives and sulfonamides), inflammatory bowel disease, sarcoidosis, pregnancy and malignancy.
Dr. Robinson-Bostom says, "We have found new associations concerning the etiologies in erythema nodosum. These include hepatitis C and HIV infections, all trans retinoic acid, echinacea herbal therapy, celiac disease as well as carcinoid syndrome."
The list of causes of primary lobular panniculitis is long and includes sclerema neonatorum (rare), pancreatic fat necrosis, subcutaneous fat necrosis of the newborn, alpha-1 antitrypsin deficiency, post-steroid-, cold-, foreign body/factitial-, cytophagic histiocytic- and neutrophilic panniculitis.
"In pancreatic fat necrosis, primary lobar panniculitis occurs in 2 to 3 percent of all patients with pancreatic disease and the panniculitis may be the only clinical presentation.
"Also, this panniculitis has been seen with acute and chronic pancreatitis, pancreatic acinar as well as with sulindac therapy.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.











