- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Potential for new dual therapy approaches in melanoma
Author(s):
A recent study suggests that genes such as ERBB2, KIT, FGFR3, and RET might be relevant in the treatment of individual patients with cutaneous melanoma.
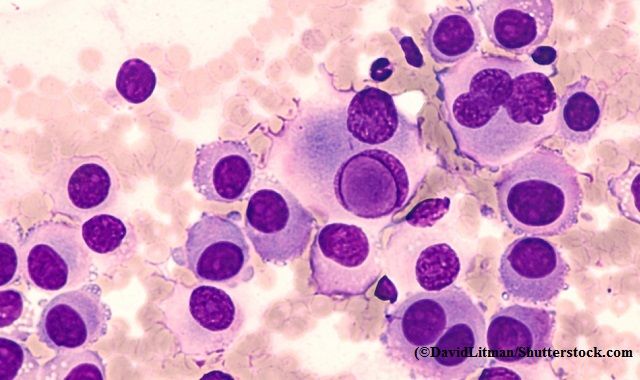
A recent study suggests that genes such as ERBB2, KIT, FGFR3, and RET might be relevant in the treatment of individual patients with cutaneous melanoma. (©DavidLitman/Shutterstock.com)
Genes such as ERBB2, KIT, FGFR3, and RET, which are targets of approved pharmacologic therapies in other cancer types but are considered atypical for cutaneous melanoma, might be relevant in the treatment of individual patients, a study published in Cancer suggests.i
The BRAF/MEK inhibitor combination is a recognised treatment option for patients with activating BRAF mutations at position 600, but for patients with melanomas with other oncogenic genetic aberrations, effective signalling pathway inhibitors have not yet been approved.
Patients who respond to BRAF/MEK inhibitors usually develop resistance within 9 to 12 months, so identifying additional, potentially actionable genomic alterations, allowing the individualization of inhibitor combinations as treatment, would be beneficial by enabling them to receive a dual therapy regime.
German researchers analysed 45 primary melanomas and 91 metastatic melanomas from 92 patients receiving treatment at the University Hospital in Würzburg, using a self-designed melanoma panel including more than 50 genes focused on the most relevant genetic alterations in melanoma and on genes that affect signaling pathways and thus can be targeted by pharmacologic inhibitors.
The panel was developed based on information derived from the previous analyses of the exomes and genomes of several hundred melanomas to identify the most frequently mutated genes and potentially relevant melanoma oncogenes and tumor suppressors.
Genes that are untypical for melanoma were also included to detect alterations with high therapeutic relevance for patients with unknown driver mutations.
The comprehensive approach was based on targeted DNA sequencing and supported by RNA and protein analysis.
Comparison with patient-matched blood samples allowed the researchers to detect actionable somatic mutations, copy number variations (CNVs), and germline variants.
Among all patients, CNVs were identified in one-third of samples and contained amplifications of druggable kinases, such as CDK4, ERBB2, and KIT.
Considering single nucleotide variants (SNVs) and CNVs, 60% of patients with metastases exhibited co-occurring activations of at least two pathways, thus providing a rationale for individualized combination therapies. Alterations in the CDK4 pathway were seen in more than 40% of patients who had metastases, including the majority of those with NRAS-mutant tumors.
Unexpectedly, 9% of patients were found to carry potentially protumorigenic germline mutations frequently affecting receptor tyrosine kinases. Two-thirds of BRAF/NRAS wild-type melanomas were found to be harbor activating mutations or CNVs in receptor tyrosine kinases such as ERBB2 and KIT.
ERBB2 expression is uncommon in melanomas, but in breast and stomach cancers, high ERBB2 levels are associated with rapid tumor growth and metastatic spread and provide the rationale for targeting ERBB2 by treatment with trastuzumab and lapatinib.ii
KIT can be targeted by small-molecule inhibitors, such as imatinib, which are approved for the treatment of gastrointestinal sarcomas with mutations in exon 11, encompassing the juxtamembrane region with amino acids 550 through 591.iii
“The combination of CNVs with activating or deleterious mutations enabled us to create a pathway matrix, which illustrates the predicted activated signaling pathways for each patient,” Silke Appenzeller, Comprehensive Cancer Center, Mainfranken, University of Würzburg, Würzburg, Germany. “Importantly, the majority of our patients harbored genomic changes, which led to at least two pathway alterations. “We propose that a targeted, deep-sequencing approach with careful consideration of oncogenic and deleterious SNVs and CNVs will help to identify patients who might benefit from a combination of BRAF/MEK inhibitors with an individually determined “inhibitor X” from the very beginning of their treatment.”
Appenzeller said that different dual-therapy regimens have been tested in preclinical mouse models with promising results.
References:
iAppenzeller S, Gesierich A, Thiem A, Hufnagel A, Jessen C, Kneitz H, Regensburger M et al. The identification of patient-specific mutations reveals dual pathway activation in most patients with melanoma and activated receptor tyrosine kinases in BRAF/NRAS wild-type melanomas. Cancer. 2018 Dec 18. doi: 10.1002/cncr.31843. [Epub ahead of print]
iiUhlen M, Fagerberg L, Hallstrom BM, et al. Proteomics. Tissue-based map of the human proteome [serial online]. Science. 2015;347:1260419.
iiiPoveda A, Garcia Del Muro X, Lopez-Guerrero JA, et al. GEIS guidelines for gastrointestinal sarcomas (GIST). Cancer Treat Rev. 2017;55:107-119.






























