- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Rethink topical antibiotic use to avoid postsurgical contact dermatitis
Knowledge of contact allergens during dermatologic surgery and in postoperative woundcare is important for all surgical and procedural dermatologists. Potential allergens found in cutaneous surgery include skin preparation substances, perioperative materials, and postoperative substances such as dressings and adhesives, an expert says.
Atlanta - Knowledge of contact allergens during dermatologic surgery and in postoperative woundcare is important for all surgical and procedural dermatologists.
Potential allergens found in cutaneous surgery include skin preparation substances such as iodine preparation, perioperative materials such as nickel-plated surgical instruments, and/or postoperative substances such as bacitracin, neomycin, dressings and adhesives, says Holly McCoppin, M.D., a dermatologist and procedural dermatology fellow at Emory University, Atlanta.
“One of the most common things we see in postoperative care is a reaction to topical antibiotics,” Dr. McCoppin says. “We typically don't use topical antibiotics on postoperative wounds anymore because of this problem. We often use topical Vaseline (Unilever) instead.”

Holly McCoppin, M.D.
Clinicians must be aware of these potential allergens in order to prevent development of allergic contact dermatitis and to recognize potential reactions early in treatment.
Postoperative reactions
Dr. McCoppin cites neomycin as one of the main culprits in the development of allergic contact dermatitis in the postoperative setting. Bacitracin is a topical antibiotic found in antibacterial and ophthalmic products. Like neomycin, it can also trigger allergic contact dermatitis characterized by redness and itching, Dr. McCoppin says. Furthermore, bacitracin can show concurrent sensitivity with neomycin.

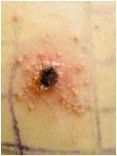
An example of allergic contact dermatitis. (Photo: Kara Braudis, M.D.)
Acutely, clinicians can apply topical steroids to help resolve an eruption of contact dermatitis. If allergic contact dermatitis has developed, it can be treated with sensitive skin care, topical steroids, and, most importantly, avoidance of the offending agent, Dr. McCoppin stresses.
“The patient basically has to avoid the allergen and the dermatitis will resolve and not return,” Dr. McCoppin says.
Glove, dressing considerations
The potential for developing allergic contact dermatitis in response to the use of topical antibiotics is heightened when there is an open wound.
“Allergic contact dermatitis is less likely to occur if the skin to which it is applied is intact,” Dr. McCoppin says.
Latex, and less commonly rubber, in surgical gloves can also cause an allergic contact dermatitis in some patients. It is important to take a history regarding previous reactions to latex prior to using latex gloves in dermatologic surgery. Similarly, for a patient with a history of latex allergy, postoperative dressings containing latex should be avoided.
Adhesives in dressings and bandages can be a source of postoperative contact allergy. Often, this is first noticed when the patient returns after surgery and a few days of postoperative care with erythema, weeping and pruritus at the site of dressing adhesives or tape.
Skin preparations such as povidone-iodine can also provoke allergic contact dermatitis, Dr. McCoppin notes.

Allergic contact dermatitis to Neosporin (Johnson & Johnson) used after punch biopsies. (Photo: Laura DeLong, M.D.)
“Putting povidone-iodine on the skin can cause a reaction,” she says. “Patients will find that they have applied it in the past and had a reaction such as itching and hives. I always ask patients if they have an allergy to it before I use it in my surgical clinic.”
Clinicians can look to alternatives such as chlorhexidine or other skin preparations in patients with known povidone-iodine allergies, Dr. McCoppin says.
Patch test approach
It may be necessary to patch-test patients who develop allergic contact dermatitis in the surgical setting if the history and exam does not reveal the culprit.
“Typically, the patient's history gives the answer, and I don't need to patch test,” she says. “If there is a repeated reaction, and I can't figure what is causing it, then I would patch-test.”
It is wise to differentiate between irritant contact dermatitis and allergic contact dermatitis, Dr. McCoppin says. There can be repeated application of adhesives that may trigger a reaction, but it is mainly an irritant reaction.
A positive patch test for allergic contact dermatitis. (Photo: Kim Neyman, M.D.)
“People may develop a skin irritation," Dr. McCoppin says. “Such a reaction is common in people who have a lot of contact with water, for instance if they are doing a lot of laundry, work in healthcare, etc.
“If surgical tape is repeatedly being applied and ripped off, the skin can become red, itchy and irritated from the repeated application of a tape adhesive,” she says. “It’s good to understand the difference between irritation and allergy. If it is an irritant, you are not having an immune response to it. You can use it again when the skin is repaired. If it is an allergen, you need to avoid the compound because each and every subsequent exposure will cause the reaction.”
Dr. McCoppin suggests clinicians verbally inform patients with allergic contact dermatitis of compounds that are safe to use in order to prevent flares of allergic contact dermatitis, as well as giving patients a takeaway list of what they can and cannot use.
“If it is not on the list, they should not use it,” Dr. McCoppin says.
As a general rule, patients should try to use compounds, such as moisturizers or lotions, that are free of fragrances or dyes because those moisturizers or lotions are less likely to have preservatives or additives, and therefore less likely to cause allergic contact dermatitis, according to Dr. McCoppin.
Disclosures: Dr. McCoppin reports no relevant financial interests.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.











