- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Slow motion: Mohs surgeons tackle difficult-to-demarcate melanomas
Author(s):
One Mohs surgeon is successfully using the "slow Mohs" technique to treat rare melanomas that are large, invasive and amelanotic.

Key Points
Delray Beach, Fla. - "Slow Mohs" is the best option for difficult-to-demarcate melanomas, according to John Strasswimmer, M.D., a Mohs surgeon with a practice in Delray Beach, Fla.
"Most melanomas are brown and relatively straightforward to excise, using standard margins," Dr. Strasswimmer says, "but sometimes they are faint to invisible, making a determination of where to cut nearly impossible. For these amelanotic tumors, I use the 'slow Mohs' procedure."
Slow technique

"Unfortunately, in my opinion, Mohs doesn't work for melanoma," Dr. Strasswimmer says. "Freezing causes the tumors to lose the features you need to examine under a microscope."
With "slow Mohs," the surgical part of the procedure is exactly the same; only the pathology differs. The excised tissue goes to a dermatopathologist (in Dr. Strasswimmer's case, it goes to Pasqual Abenoza, M.D., of Ameripath/Dermpath Diagnostics), who places the tissue in a wax block overnight, then slices the block into paper-thin sections for microscopic evaluation while breadloafing the core to assess the depth of invasion.
"This produces the same en face margin examination that's standard in Mohs," Dr. Strasswimmer says.
"Slow Mohs" may take days, or even weeks, in the case of large or deep melanomas.
New territory
The department of dermatology, at the University of Michigan, Ann Arbor, pioneered the use of "slow Mohs" for the treatment of melanoma in situ. The technique spread to other large academic centers.
It wasn't until recently, though, that anyone in the United States used the procedure for large, invasive, amelanotic melanomas. Instead, dermatologic surgeons punted these cases to plastic or ENT surgeons.
Dr. Strasswimmer says that changed in 2007, after a plastic surgeon called him desperate for help. The surgeon had performed two large excisions and repairs on a patient's glabellum, failing to remove a tumor that stretched 10 cm by 10 cm.
"In my Mohs surgery fellowship, I learned to accept the most challenging surgical cases. For this patient, I did a series of six surgeries over two weeks, then referred the patient back to the plastic surgeon for reconstruction," Dr. Strasswimmer says.
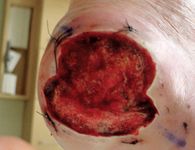
Since then, he has performed "slow Mohs" on two additional patients. The second patient had a 15 cm by 15 cm melanoma on a temple; it required seven sessions. The third patient had a deep tumor (7.2 mm) on the heel and was initially referred for amputation.
After "slow Mohs," all of the patients remained cancer-free with good function and cosmetic results at two years. The foot patient received a skin graft and now walks normally.
Academic oculoplastic surgeons in London have echoed these results. In a Jan. 2009 article published in Dermatologic Surgery, they describe early cure rates using "slow Mohs" surgery for 14 cases of periocular malignant melanoma. The tumors were smaller than those undertaken by Dr. Strasswimmer, but the procedure was identical, he says.
"The surgeons showed an excellent cure rate and excellent tissue preservation," Dr. Strasswimmer says. "Two cases of recurrence were managed with local excisions."
In determining the size of margins to remove, Dr. Strasswimmer considers the depth of the tumor and how much function needs to be preserved. In one case, he removed a portion of the tarsal plate of the eyelid but left the conjunctiva intact and free of tumor. This allowed an oculoplastic surgeon to perform complete reconstruction.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.











