- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Subcutaneous Nodules Misdiagnosed as Pilomatricoma
Author(s):
When children present with nodules, several diagnoses should be considered, including pilomatricoma, vascular tumors, and fibrous tumors.
Pilomatricoma is a common tumor in children but is often misdiagnosed. Researchers reviewed 4 cases of children with subcutaneous nodules for misdiagnoses and discussed common characteristics of pilomatricoma.1
David A Litman/AdobeStock
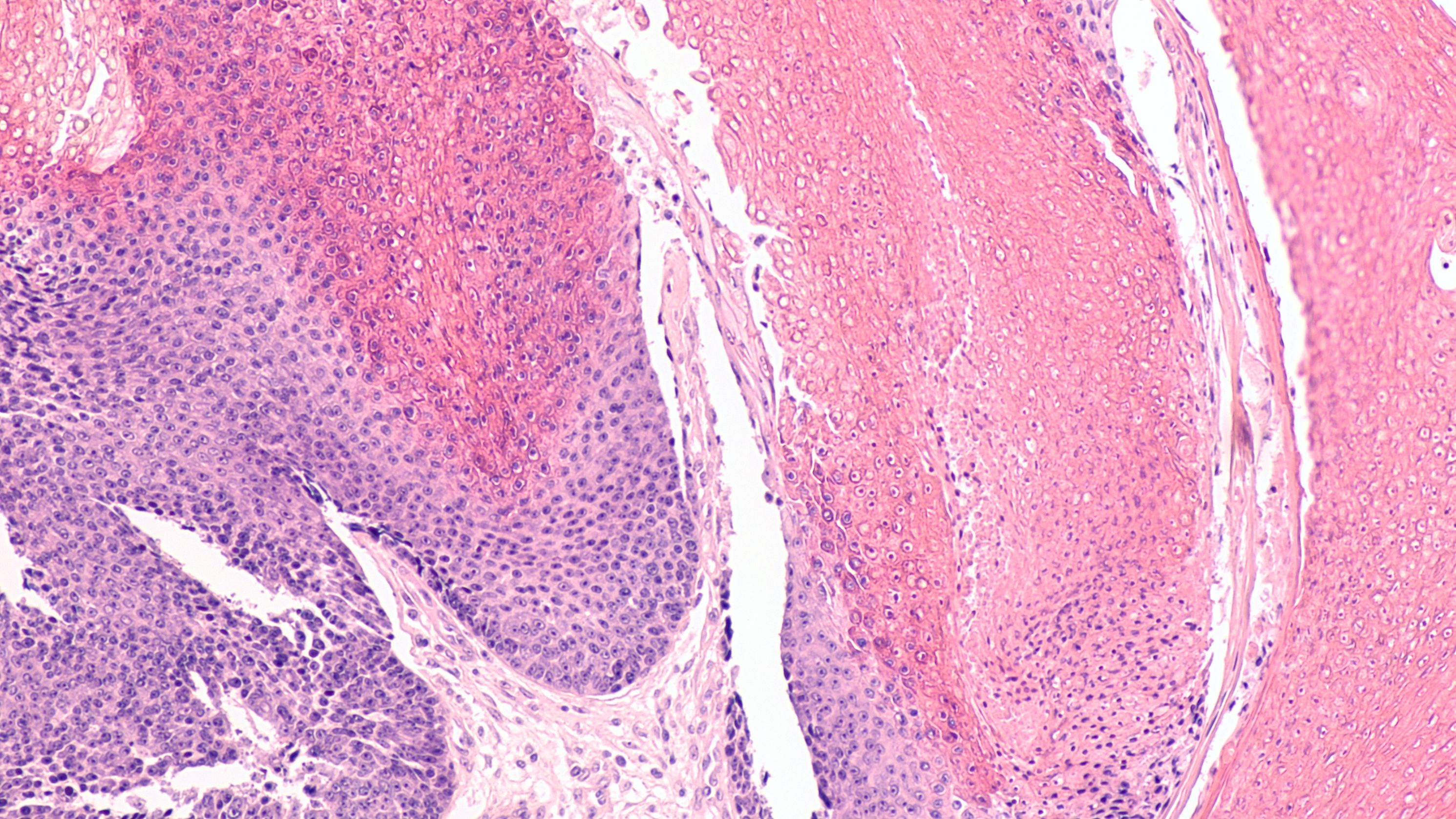
In the first 2 cases, nodules were incorrectly diagnosed before being reexamined and confirmed to be pilomatricoma. The first case was a 7-year-old boy with a red mass that had been on his scalp for 2 weeks. Examination showed a .6-cm-sized hemispherical, soft mass with a hidden firm nodule beneath. It was initially misdiagnosed aspyogenic granuloma. Excision and histopathological examination revealed basophilic cell and shadow cells and confirmed pilomatricoma.
In the second case, an 8-year-old boy with a red mass on his face for 3 months was examined. The 1-cm-sized mass with a hidden firm nodule underneath had been misdiagnosed as infantile hemangioma. Dermoscopic examination revealed an irregular white structureless area and dendritic vessel on a red background. Excision and histopathological examination confirmed pilomatricoma. Neither of these cases had a history of local trauma.
Cases 3 and 4 were initially diagnosed as pilomatricoma but further examination revealed other diagnoses. A 21-month-old girl had a red mass on her breast that was increasing rapidly over 7 months. Histopathological examination of the tumor revealed a 2-phase pattern composed of “eosinophilic regions with spindle cells containing richly cellular and basophilic regions with small round or oval cells arranged around the blood vessels. Immunohistochemically, the tumor cells were positive for SMA and negative for CK (AE1/AE3), CD68, S100, CD34, CD31, ALK, Catenin, Myogenin, Desmin, and CD99.” The findings, combined with clinical and pathological manifestations, led to a diagnosis of infantile myofibroma. Following treatment with oral propranolol the tumor did not continue to grow.
A 13-month-old girl who had been vaccinated against Bacille Calmette-Guérin (BCG) developed a nodule in her armpit that was present for 10 days. The 1 cm by 1.5 cm subcutaneous nodule was tough, well-defined, and movable. Initially diagnosed as pilomatricoma, ultrasound revealed a “hypoechoic nodule in the subcutaneous layer with clear boundary and multiple hyperechoic calcifications.” A lymph node biopsy showed lymphadenitis, leading to a diagnosis of BCG-associated lymphadenitis. The nodule narrowed following treatment with rifampicin and isoniazid.
Pilomatricoma is a slow-growing tumor with features that include reddish homogeneous areas, irregular whitish structures, dotted vessels, or linear-irregular vessels. Ultra-high-frequency ultrasonography can be helpful in diagnosing pilomatricoma, revealing echogenic foci (calcifying) and hypoechoic rim. Surface skin above pilomatricoma can be skin-colored, which may result in a misdiagnosis of epidermal cyst.
Determining the correct diagnosis is important because treatments vary depending on disease.
Reference
- 1. Sun J, Fu LB, Xu JS, Han XF, Wei L. Confused subcutaneous nodules in children: Differential diagnosis of pilomatricoma in children. J Cosmet Dermatol. 2023; 00: 1-5. doi:10.1111/jocd.15868
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.











