- Case-Based Roundtable
- General Dermatology
- Eczema
- Chronic Hand Eczema
- Alopecia
- Aesthetics
- Vitiligo
- COVID-19
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Wound Care
- Rosacea
- Psoriasis
- Psoriatic Arthritis
- Atopic Dermatitis
- Melasma
- NP and PA
- Skin Cancer
- Hidradenitis Suppurativa
- Drug Watch
- Pigmentary Disorders
- Acne
- Pediatric Dermatology
- Practice Management
- Prurigo Nodularis
- Buy-and-Bill
Article
Targeted therapy and adoptive T-cell therapy offer alternatives to immunotherapy
Other strategies such as adoptive T-cell therapy are initiated when immune therapies fail to stop disease progression in advanced melanoma.
Despite the existence of new immune therapies, some patients with advanced melanoma have disease which continues to progress, forcing clinicians to look at treatment strategies beyond immunotherapy, according to a medical oncologist at Princess Margaret Cancer Center in Toronto, Canada.
Speaking at the 9th Canadian melanoma conference, Marcus Butler, M.D., discussed the efficacy of immune therapies such as ipilimumab, pembrolizumab, and nivolumab and developments in adoptive immunotherapy in the treatment of advanced disease.
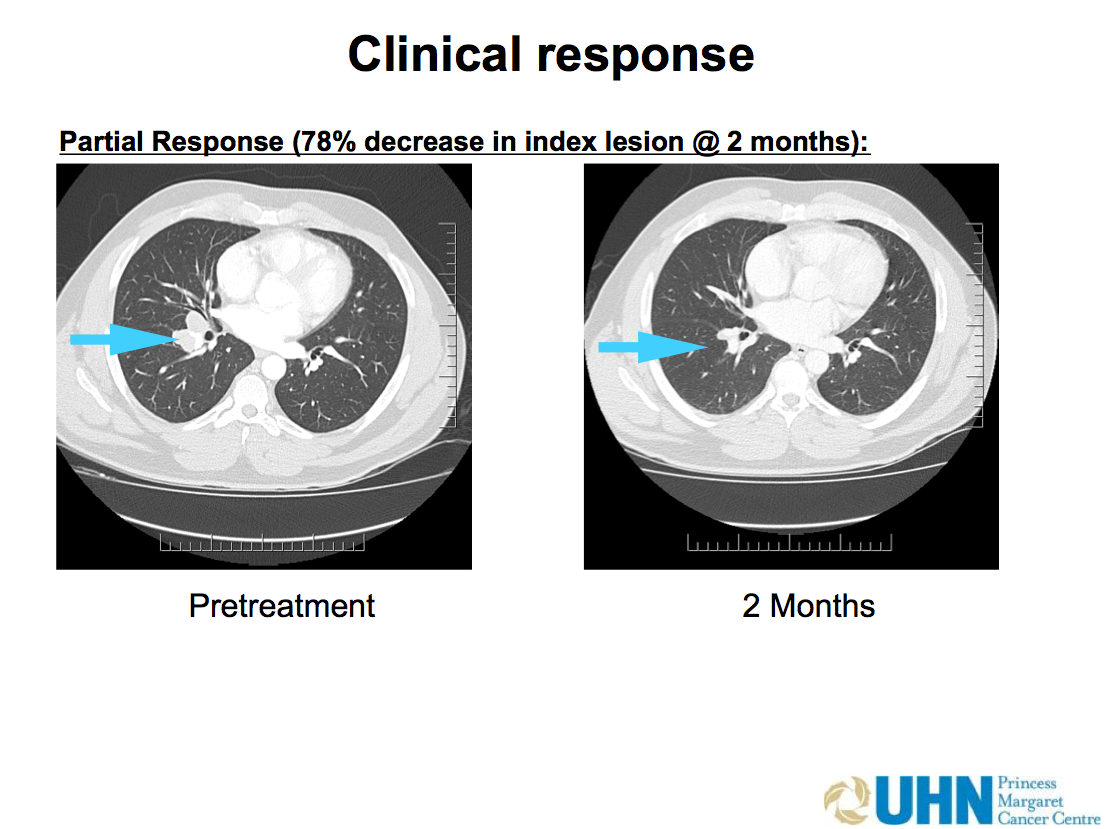

Photo credit: Marcus Butler, MD
Multiple methods
"There are multiple methods for using the immune system to fight cancer," says Dr. Butler in an interview with Dermatology Times. "The short answer is that we don't have a perfect biomarker to tell us who will respond [to immune therapies] and who will not. Many of us feel like what we have to do is identify who will respond right off the bat with single agents that don't have a lot of side effects and [identify] which patients may require combination therapy that has the potential for more side effects."
Using targeted therapy will require different drugs because of the different mutations present, and there have been some challenges with achieving response with targeted therapy that targets other genes outside of the BRAF gene, explains Dr. Butler.
NEXT: PDL 1 Expression
PDL1 expression

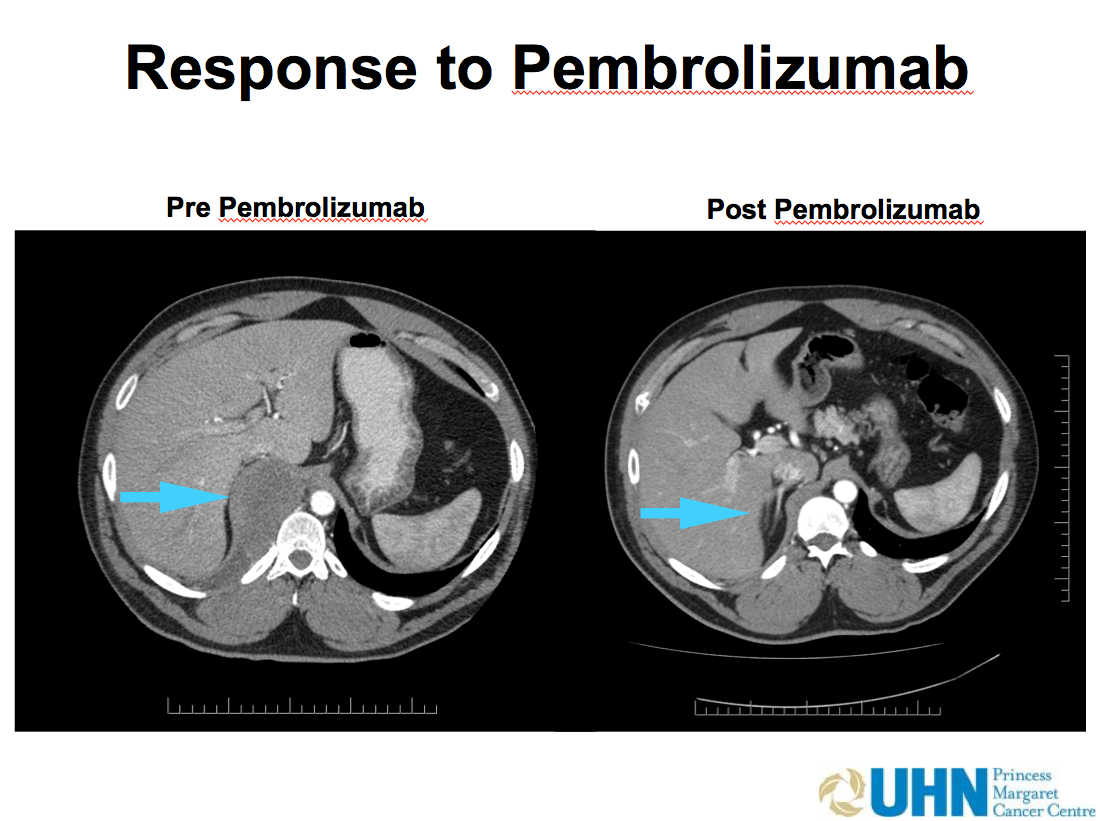

Photo credit: Marcus Butler, MD
Positive PDL1 expression of a tumor suggests greater benefit from drugs like pembrolizumab and nivolumab, but PDL1-negative patients can still have a meaningful response to the agents, notes Dr. Butler.
Clinicians are looking for biomarkers to assist them in determining if single agent therapies or a combination of therapies is an appropriate treatment strategy, says Dr. Butler. "That is an active area of research to distinguish populations," says Dr. Butler.
Some patients require jumpstarting their immune responses to a tumor. "The checkpoint drugs are not [always] able to unleash that response," says Dr. Butler. The approach in such situations has been to implement adoptive T-cell therapy, where immune cells are grown in culture and infused back to patients as a therapy to induce responses, explains Dr. Butler.
NEXT: TIL protocol
TIL protocol

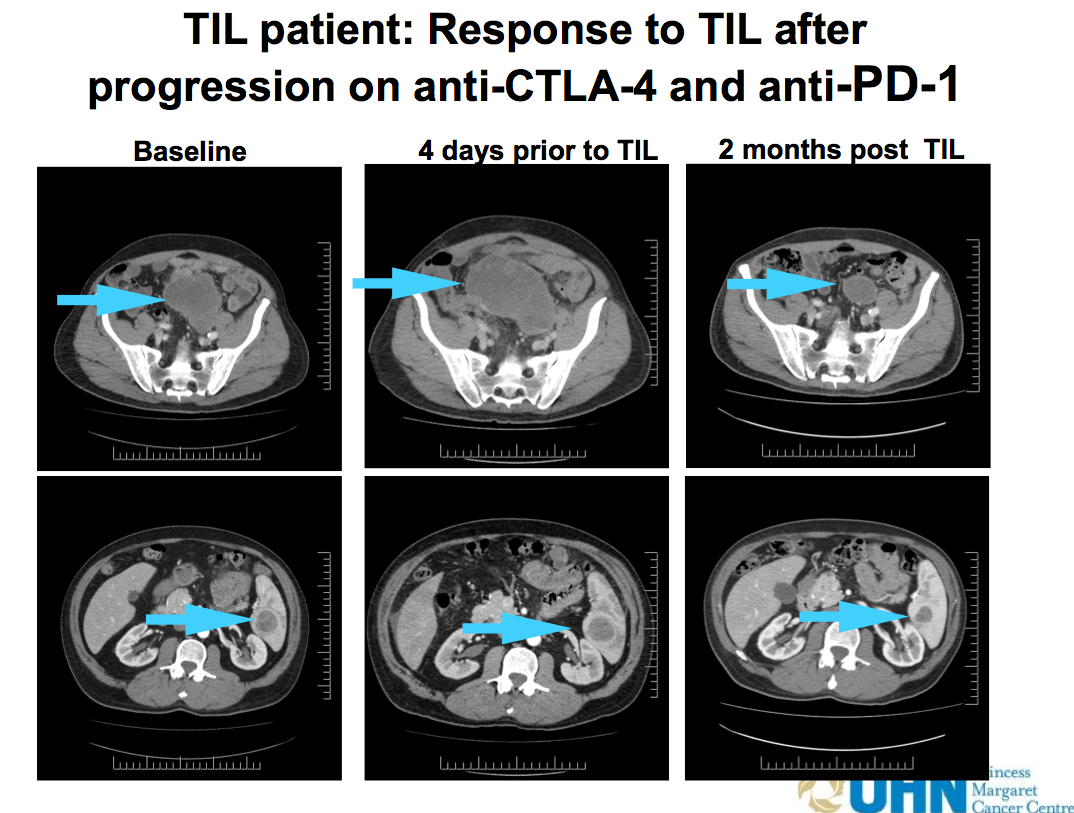

Photo credit: Marcus Butler, MD
"One of the difficulties with the TIL (tumor infiltrating lymphocytes) protocol is that patients require high doses of chemotherapy prior to the infusion of T-cells," says Dr. Butler. "Patients are also treated with IL-2 after the T-cell infusion."
Dr. Butler and colleagues have modified the dose of IL-2 at Princess Margaret Cancer Center in Toronto in comparison to doses given at other centers in North America where the TIL protocol is being implemented.
In terms of durability of response, Dr. Butler says that immune therapy can be long-lasting, but the lasting effect of the PD1 checkpoint inhibitors has not yet been established because the drugs are relatively new.
Some groups with the TIL protocols have shown lasting response, typically years, in about 20% of patients, but Dr. Butler says that the required use of high-dose chemotherapy as part of the protocol means that it will likely be reserved as a salvage regimen.
NEXT: References
References: Dr. Butler has served on advisory boards for Merck, BMS, and Novartis.





