- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Atopic dermatitis patients need better disease control
Author(s):
Adult patients with moderate-to-severe atopic dermatitis who were treated with systemic agents, including cyclosporine, azathioprine, mycophenolate mofetil, methotrexate or cyclophosphamide, reported a high level of disease-related burden despite those treatments, says a recent study.

Adult patients with moderate-to-severe atopic dermatitis who were treated with systemic agents, including cyclosporine, azathioprine, mycophenolate mofetil, methotrexate or cyclophosphamide, reported a high level of disease-related burden despite those treatments, according to research published in the Annals of Allergy, Asthma and Immunology.1
RELATED: Atopic dermatitis pipeline full of potential
They not only reported severe disease symptoms, but also recurrent ares, impaired quality of life, reduced work productivity and compromised daily activities.
“The study period was prior to the availability of dupilumab (Dupixent, Sano Regeneron) in moderate-to-severe atopic dermatitis. However, it shows that the standard of care with currently available topical, oral systemic and phototherapies is clearly inadequate and that there is a need to improve control of atopic dermatitis in the United States,” says the study’s senior author Jonathan I. Silverberg, M.D., Ph.D., MPH, associate professor of dermatology, medical sciences and preventive medicine at the Feinberg School of Medicine, Northwestern University, Chicago.
Researchers conducted a longitudinal, prospective, observational study of atopic dermatitis patients who had been diagnosed in the last five years and had been prescribed systemic immunosuppressants, systemic corticosteroids or phototherapy. Participants completed a baseline paper survey, followed by web-based surveys at three, six, nine and 12 months, as well as shorter monthly web-based surveys in between.
Of the 801 adult participants analyzed, more than 66% said they had been diagnosed at 21 years or older.
“While 66% is a little on the high side, it is important to note that adult-onset atopic dermatitis is more common than many clinicians recognize. A recent meta-analysis found that approximately one in four adults with atopic dermatitis report adult onset of their disease,” Dr. Silverberg tells Dermatology Times.
RELATED: Atopic dermatitis treatment hurdles
More than 26% of adults reported having severe atopic dermatitis.
Most participants (63.6%) reported using topical corticosteroids in the last month, while 11.4% used systemic corticosteroids and 5.1% had used systemic immunosuppressants in the last month, according to the 12 months prior to the baseline survey.
More than 81% of patients indicated they had experienced at least one are over the past month, according to the baseline monthly data.
“Regardless of baseline [atopic dermatitis] severity, and despite having received systemic agents in the past six months, a significant proportion of patients (38.3%) had not experienced remission in the prior 12 months,” the authors write.
Data from the Patient-Oriented Eczema Measure (POEM), a seven-item measure of symptom frequency in the past week, revealed that 57.6% of participants reported moderate to very severe symptoms in the short term. More than 34% of patients indicated they experienced one to four days of disrupted sleep in the last week. Severe atopic dermatitis patients fared worse in those two outcomes.
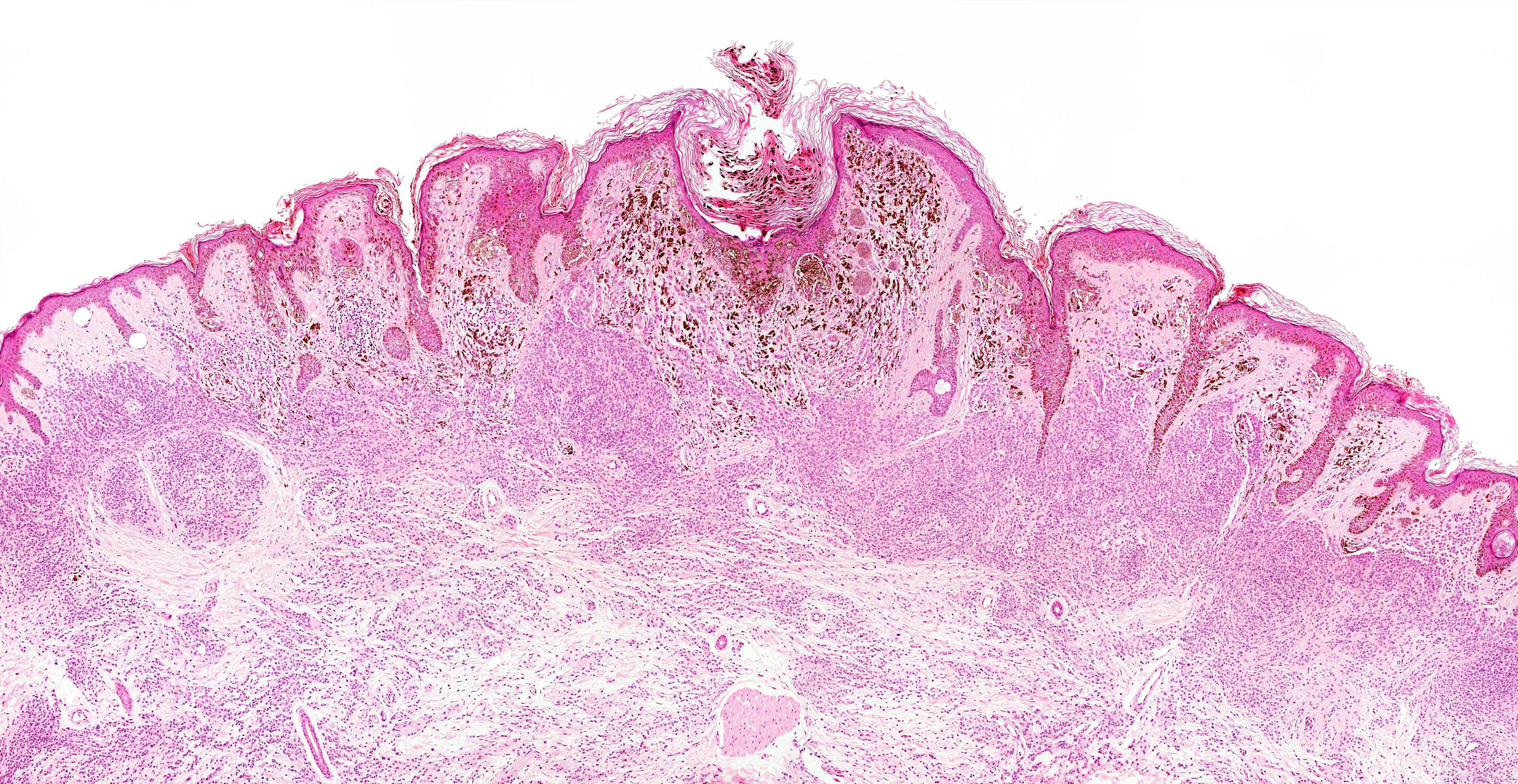
RELATED: Molecular mechanisms that disrupt the epidermal barrier
Nearly 44% indicated that atopic dermatitis moderately to extremely impacted their quality of life. The e ect was worse when patients were experiencing ares, more frequent ares or severe disease.
Nearly 79% of working participants reported missing work due to atopic dermatitis an average 7.1 hours in the last seven days.
“Despite using systemic treatments, patients with severe and currently aring AD were similarly dissatisfied with the medications that they were taking for their [atopic dermatitis] …,” according to the authors. “These results suggest that patients with [atopic dermatitis] have significant unmet therapeutic needs.”
References:
1. Wei W, Ghorayeb E, Andria M, et al. A real-world study evaluating adeQUacy of Existing Systemic Treatments for patients with moderate-to-severe Atopic Dermatitis (QUEST-AD): Baseline treatment patterns and unmet needs assessment. Ann Allergy Asthma Immunol. 2019;123(4):381-388.e2.