- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Imaging evolves to guide Mohs surgery
Author(s):
Combined imaging modalities may help guide choice of treatment and prevent biopsy, according to one expert.
Combined imaging modalities may help guide choice of treatment and prevent biopsy, according to one expert. (Laura Ballar - stock.adobe.com)
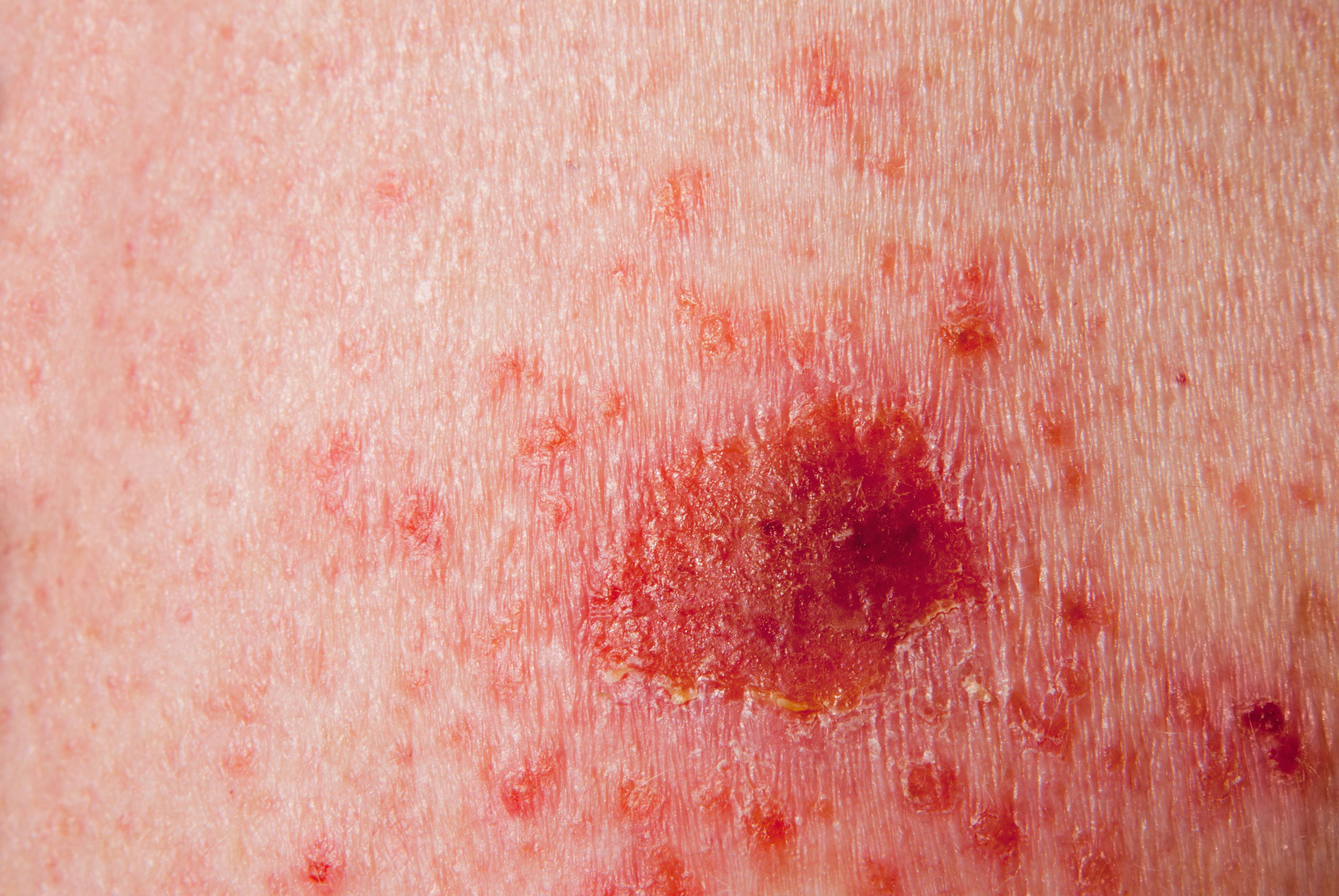
The recent impact of reflectance confocal microscopy (RCM) and optical coherence tomography (OCT) imaging modalities has been viewed as revolutionary in assisting the clinician with accurately diagnosing suspicious lesions and nonmelanoma skin cancers.
According to one expert, combining technologies is considered the next level in state-of-the-art skin cancer diagnosis and management. It may prove to be a useful adjunctive tool to guide Mohs surgery as well as other nonsurgical treatments.
Mohs surgeons are currently using both RCM and OCT imaging techniques to map out the margins of nonmelanoma skin cancers on patients before the start of surgery. These technologies help them determine the lateral spread of the tumor under investigation, says Milind Rajadhyaksha, Ph.D., Dermatology Service, Department of Medicine, Memorial Sloan Kettering Cancer Center, New York, who recently spoke at the annual ASLMS conference in Denver.
Once the surgeon has a sense of the lateral spread, they then often have a general sense for the depth of the tumor and can better estimate how much tissue needs to be excised, he says.
“Following the example of current therapies used in Europe, some Mohs surgeons in the United States are also beginning to treat these superficial lesions with nonsurgical approaches, such as topical therapy or photodynamic therapy (PDT) or even with laser ablation,” Dr. Rajadhyaksha says. “The imaging and particularly the combination of the technologies can help them guide the choice of treatment, whether to do traditional Mohs surgery or surgical excision, or perhaps they can treat the tumor with topical noninvasive therapies and avoid biopsy.”
Reflectance confocal microscopy creates images at a shallow depth giving the clinician nuclear and cellular level morphologic detail of the targeted lesion, and it has a sensitivity of approximately 80% to 95% and a specificity of 65% to 80%.
The faster OCT device in contrast creates deeper images that allow the clinician to quickly view the structural level morphology and assist in determining the depth and the deep margins of the lesion under scrutiny. In addition, it has a sensitivity of 79% to 96% and a specificity of 58% to 96% percent.
“The confocal microscopic imaging provides a higher resolution than those attainable with OCT, but the OCT images go deeper than confocal microscopy, and it’s the combination of both of these modalities that can really serve as an excellent imaging tool. Moreover, the combination RCM/OCT device is also proving to be very promising as an adjunctive procedure to Mohs surgery,” Dr. Rajadhyaksha says.
Still in early technical development, Dr. Rajadhyaksha and his collaborating team, which includes Nicusor Iftimia, B.Sc., M.S., Ph.D., Physical Science, Inc., and Mr. William Fox, Caliber Imaging and Diagnostics, recently engineered two prototype combination RCM/OCT devices that are currently under investigative research at Memorial Sloan Kettering Cancer Center.
In the clinical setting, the combination of these two imaging technologies in a single device helps the surgeon to get a better sense for the depth and the deep margins, for example in cases where the tumors are superficial or early nodular (i.e., the tumor depth is within 300-400 microns).
“In the preliminary data we have with our prototype devices, the in-vivo and ex-vivo imaging approach using the combination RCM/OCT device can be very useful to help guide Mohs surgery as well as to help guide the choice of other nonsurgical treatment modalities,” Dr. Rajadhyaksha says.
The combined RCM/OCT device may take a few more years to commercialize. However, according to Dr. Rajadhyaksha, the promising impact the combination device can have in the treatment and management of this patient population is significant.
Although the dermatoscope remains the right-hand diagnostic tool for skin cancer screening in the dermatologic practice, combination RCM and OCT technologies will bring the advantages of both technologies into one single device, Dr. Rajadhyaksha says, and this may help to prevent biopsy procedures.
Disclosures:
Dr. Milind Rajadhyaksha is a former employee of Caliber Imaging and Diagnostics (formerly, Lucid Inc.), the company that manufactures and sells the VivaScope confocal microscope. He owns equity.
The VivaScope is the commercial version of an original laboratory prototype that was developed by Dr. Rajadhyaksha when he was at Massachusetts General Hospital, Harvard Medical School.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.