- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
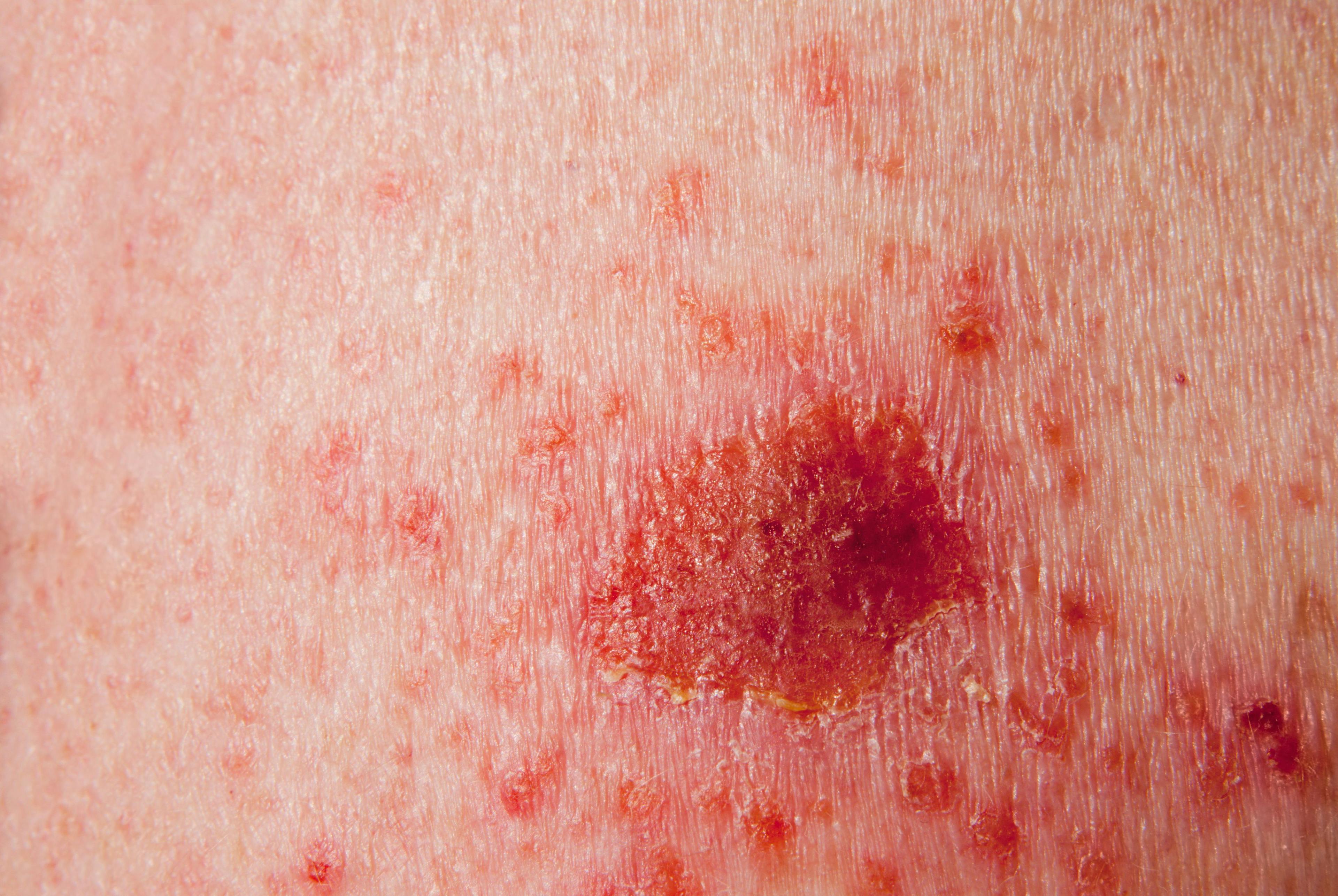
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Effect of Joint Pain on Analgesic Use in Patients with Psoriasis
Author(s):
In a recent study from the Journal of the American Academy of Dermatology, investigators assessed symptoms, disease burden, and use of analgesics in patients with or without psoriatic arthritis.
Patients with psoriasis, especially those with concomitant psoriatic arthritis (PsA), use analgesics more frequently than the general population, according to a cross-sectional study in the Journal of the American Academy of Dermatology.
“We knew from previous studies that patients with psoriasis have a higher use of analgesics than the general population, but the reason had not been well described,” said principal investigator Nikolai Loft, MD, PhD, a senior researcher in dermatology and allergy at Gentofte University Hospital in Copenhagen, Denmark.
The reason for this increased use of analgesics is likely due to increased joint pain, according to study.
“Joint pain is common among patients with psoriasis—both those with psoriatic arthritis and those without,” Loft told Dermatology Times®. “This joint pain is associated with use of analgesics and impaired general health, whereas skin symptoms are associated with worse quality of life (QOL) to a higher degree than the affected body surface.”
To expand the knowledge base on this subject, investigators aimed to assess the symptoms, disease burden, and use of analgesics in patients with and without PsA.
The study population from the Danish Skin Cohort comprised of 4,016 patients with psoriasis, of whom 21.1% (n = 847) also had PsA. These patients were compared to a control group from the Danish Skin Cohort of 3,490 individuals without psoriasis.
The mean age of the general population was 54.7 years vs 59.4 years in the psoriasis population. Additionally, 55% of the comparison group were women vs 56% of psoriasis group.
At the time of self-assessment, 47% of psoriasis patients reported mild disease, 25.4% moderate disease and 27.6% severe disease.
Symptoms, general health, and analgesics usage were assessed in all participants. General health was measured via EuroQoL 5 Dimensions 5 Levels (EQ-5D-5L), which encompasses 5 areas: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
Psoriasis located on the face, hands, genitals, and feet was linked to itch and skin pain. Patients with psoriasis, PsA, itch, skin pain, and/or joint pain had worse general health, according to the study.
The percentage of the general population reporting moderate to severe skin pain, joint pain, and itch was 7%, 35%, and 10%, respectively.
In contrast, moderate to severe itch was reported by 34% of psoriasis patients with PsA and 30% without (P = 0.022); moderate to severe skin pain by 30% and 21%, respectively (P < .0001); and moderate to severe joint pain by 69% and 45%, respectively (P < .0001).
General health was worse in patients with psoriasis compared to the general population across all psoriasis severities: .86 vs .90 with EQ-5D-5L, respectively (P < 0.001); also, significantly worse in patients with psoriasis and PsA than those without PsA: .80 vs .87 (P < 0.001).
Joint pain had the highest impact on worsening general health. Symptoms originating from the skin and joints were associated with increased risk of reporting any problems in all EQ-5D-5L domains, with joint pain showing the strongest link to most domains.
As for disease burden, 47.6% of psoriasis patients reported no effect on the Dermatology Life Quality Index (DLQI), 30.3% reported a small effect, 12.7% reported a moderate effect, 8.3% reported a very large effect, and 1.2% reported an extremely large effect at the time of assessment.
There was no difference in DLQI among patients with PsA and those without PsA across psoriasis severities. However, patients with a higher percentage of affected body surface area (BSA) typically reported a higher impact on DLQI, with a weak to moderate correlation between BSA and DLQI.
In addition, skin pain and itch showed moderate correlations with DLQI, while joint pain showed a negligible correlation.
Patients with more-severe skin symptoms also reported a significantly higher impact on QOL, independent of psoriasis severity.
The number of dispensed prescriptions of the analgesic medication paracetamol (acetaminophen), nonsteroidal anti-inflammatory drugs, opioids and gabapentin/pregabalin were obtained for study participants through an individual-level linkage with the nationwide Register of Medicinal Products Statistics, reported the investigators.
Patients with psoriasis used more analgesics than the general population and patients with PsA used more analgesics than those without PsA. However, there was no connection between the extent of psoriasis and use of any of the examined analgesics. Prescription of several analgesics was associated with increasing severity of symptoms from both the skin and joints.
Opioid use within 12 months occurred in 9% of the general population, 14.2% of psoriasis patients without PsA, and 22.7% of psoriasis patients with concomitant PsA.
For psoriasis patients without PsA, 12.7% with mild or no itch had used opioids in the last 12 months at the time of the study and 12.9% for skin pain (P = .001). For those with severe itch and pain the corresponding percentages were 19.4% and 19.3% (P < 0.001).
The study results stated that only joint pain was associated with use of analgesics (odds ratio (OR) = 3.72; 95% confidence interval (CI): 2.69 to 5.14 (P = .0001).
“We anticipated that patients with psoriasis would use analgesics more frequently for symptoms of both the joint and the skin, rather than simply for joint pain,” Loft said. “Treating physicians should be aware of symptoms, including those from the joint and the skin.”
Disclosure:
Loft has been an honorary speaker for Eli Lilly and Company and Janssen-Cilag.
Reference:
Loft N, Nguyen TT, Kristensen LE, et al. Disease burden, symptoms, and use of analgesics in patients with psoriasis with or without psoriatic arthritis: a cross-sectional study. J Am Acad Dermatol. 2022;86:590-597. doi:org/10.1016/j.jaad.2021.07.028

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.