- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Genital Skin Cancers and Lichen Sclerosus
Author(s):
Many studies have investigated the associations between lichen sclerosus and vulvar and penile SCCs, as well as genital melanomas.
Due to feelings of shame, stigma, and discomfort that can accompany genital cancer,1 it is important for clinicians to encourage patients to report any unusual signs and symptoms they may be experiencing in order to quickly diagnose and treat before the cancer becomes more advanced.
Vaginal melanomas account for approximately 3% of vaginal cancers,2 with vulvar melanoma accounting for approximately 1% to 2% of all melanomas.3 Even more rare, penile melanomas account for 0.18% of all melanomas and only 0.7% of all penile cancers.4
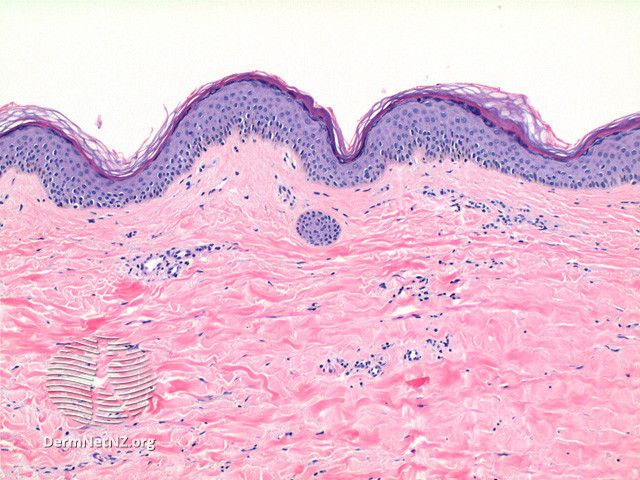
One dermatologic comorbidity that may be associated with skin cancers of the genital region is lichen sclerosus. Several studies5-7 have established associations between lichen sclerosus and vulvar and penile SCCs, as well as genital melanomas; although it is noncancerous, an estimated 4% of patients with lichen sclerosus will develop cancer of the vulva.8
Study Findings: Penile Melanomas and Lichen Sclerosus
In a study9 published in Skin Health and Disease, researchers found that genital lichen sclerosus (GLSc) was present in 82% of penile melanoma cases. To explore the relationship between male GLSc and penile melanoma, researchers reviewed all relevant cases from a tertiary urology and male genital dermatology service. The retrospective analysis included patients with a penile melanoma diagnosis and available histopathology to review. All patients had been seen between 2011 and 2022.
Clinical records and photographs were first reviewed by a team of 2 dermatologists; 2 histopathologists conducted independent reviews of patient histopathology and features of GLSc. Eleven patients with penile melanoma were identified, and researchers collected clinical and demographic information relevant to the study, including age at diagnosis; ethnicity; features of GLSc; and melanoma subtype, stage, and mutation when applicable.
In 9 of the 11 cases, or 82% of patients, GLSc was present in histopathology. These patients were found to have clinical features of male GLSc. Prior to this study, there had only been 3 documented cases of GLSc and penile melanoma comorbidity.
According to the study, “In addition to being under-recognised clinically, GLSc in the context of [melanoma] might also be under-recognised histologically,” according to Dear et al. “The histopathological confirmation of the presence of LSc in 9 out of 11 men with penile melanoma seen at our tertiary centre does not prove a causative relationship between GLSc and penile melanoma but is suggestive. We theorise that this is related to chronic melanocytic distress created by LSc. Our findings have implications for the prevention, early diagnosis, management, and follow-up of MGLSc [male GLSc].”
Lasting Impacts of Lichen Sclerosus
In a cohort of adult females who had received a histologically confirmed diagnosis of vulvar lichen sclerosus (VLS) in childhood or adolescence, more than half (51.9%) reported long-term lasting impacts to their overall quality of life and sexuality, according to a study10 published in Acta Obstetricia et Gynecologica Scandinavica.
According to Morrel et al, VLS occurs in around 1 in 900 young females and is commonly diagnosed in prepuberty. Despite this, they note that there is limited research exploring the extent of the condition’s impacts into adulthood.
Investigators identified all histological data regarding vulvar biopsies classified as lichen sclerosus from the Dutch Pathological-Anatomical National Computerized Archive. Biopsies had been collected from juvenile female patients between 1991 and 2015. Investigators then requested tissue samples from pathology laboratories in the Netherlands. All biopsies were reviewed by a team of pathologists, a gynecopathologist, and a dermatopathologist, excluding inconclusive biopsies, poor tissue samples, and samples featuring concomitant lesions.
Once determining that samples belonged to patients who were 18 years or older as of January 1, 2021, investigators went through the process of identifying the patients associated with the samples and acquiring informed consent. Participants (n = 81) were asked to complete an online questionnaire, including questions specific to the Dermatology Life Quality Index (DLQI), Skindex-29, Female Sexual Function Index, and Female Sexual Distress Scale-Revised, of which 80 participants completed all 5 parts. Participants also answered questions relative to their past and present experiences with VLS.
According to the results of the questionnaire, 51.9% of respondents reported VLS having some degree of impact on their overall quality of life, with 6.2% reporting a large quality-of-life impact in accordance with the DLQI. Skindex-29 responses revealed that VLS had impacted the quality of life of 30.9% of respondents, with 9.9% having a severe impact. Of the respondents, more than half reported sexual dysfunction (51.9%) and sexual distress (53.7%).
Moving Forward
Respondents were then able to respond openly about their experiences with VLS. One respondent wrote, “The diagnosis was made when I was a teenager, at an age when you want to go out and discover the world, just like one’s peers. The lichen sclerosus always held me back.” Respondents also reported frequent urinary tract infections, pain during intercourse, concerns about risks of developing vulvar cancer, concerns about whether delivery of a child would be impacted by the condition, and dissatisfaction with their appearance.
“Despite the current advice that females of any age with VLS should be offered surveillance and maintenance treatment, more than half (54%) of the participants were not under surveillance,” according to study authors Morrel et al. “The impact on QoL [quality of life] and sexual well-being in this relatively young study group, as assessed by available instruments, seems to be more favorable then previously reported for VLS but correlates strongly with current symptoms. Over half of the participants had suffered from symptoms within the past year.... This study is hopefully a starting point for further research on this topic, the ultimate goal being to improve care and counseling of these young patients from time of diagnosis onwards.”
References
1. Vaginal cancer: coping with treatment. Cancer.Net. September 2022. Accessed September 14, 2023. https://www.cancer.net/cancer-types/vaginal-cancer/coping-with-treatment.
2. Vaginal melanoma. Cancer Research UK. Updated March 2, 2022. Accessed September 14, 2023. https://www.cancerresearchuk.org/about-cancer/vaginal-cancer/types-grades/melanoma#:~:text=Vaginal%20melanoma%20is%20a%20rare,lower%20third%20of%20the%20vagina.
3. Falcicchio G, Vinci L, Cicinelli E, et al. Vulvar malignant melanoma: a narrative review. Cancers (Basel). 2022;14(21):5217. doi:10.3390/cancers14215217
4. Jabiles AG, Del Mar EY, Perez GAD, Vera FQ, Montoya LM, Deza CMM. Penile melanoma: a 20-year analysis of six patients at the National Cancer Institute of Peru, Lima. Ecancermedicalscience. 2017;11:731. doi:10.3332/ecancer.2017.731
5. Sim SJY, Dear K, Mastoraki E, et al. Genital lichen sclerosus and melanoma; a systematic review. Skin Health Dis. 2022;3(2):e198. doi:10.1002/ski2.198
6. Lewis F. Dermatoses of the female genitalia. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer T, eds. Rook’s Textbook of Dermatology. 9th ed. Wiley-Blackwell; 2016:112.6-112.9.
7. Bunker CB, Watchorn R. Dermatoses of the male genitalia. In: Griffiths C, Barker J, Bleiker T, eds. Rook’s Textbook of Dermatology. 10th ed. Wiley-Blackwell (in press).
8. Vulvar cancer: risk factors and prevention. Cancer.Net. Updated May 2022. Accessed September 14, 2023. https://www.cancer.net/cancer-types/vulvar-cancer/risk-factors-and-prevention#:~:text=Lichen%20sclerosus.,lichen%20sclerosus%20develop%20vulvar%20cancer.
9. Dear K, Kravvas G, Sim S, et al. Primary penile melanoma and genital lichen sclerosus. Skin Health Dis. Published online August 12, 2023. doi:10.1002/ski2.274
10. Morrel B, van der Avoort IAM, Ewing-Graham PC, et al. Long-term consequences of juvenile vulvar lichen sclerosus: a cohort study of adults with a histologically confirmed diagnosis in childhood or adolescence. Acta Obstet Gynecol Scand. Published online August 26, 2023. doi:10.1111/aogs.14668

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.