- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
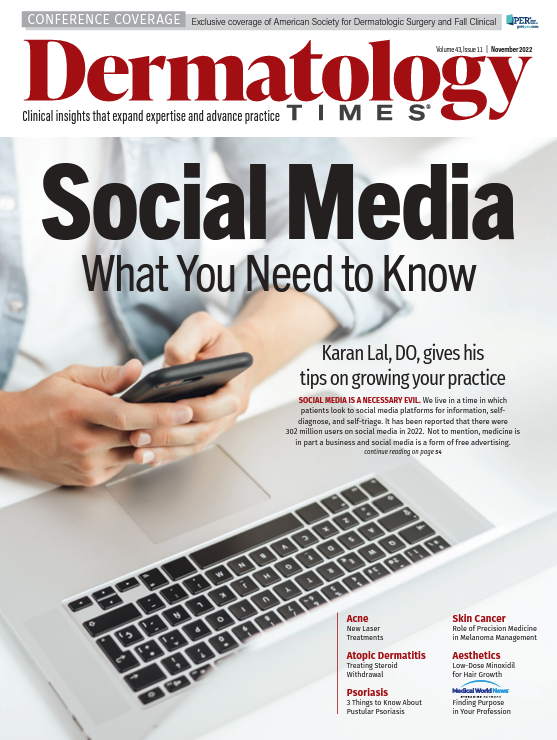
Publication
Article
Dermatology Times
How to Diagnose and Manage Alopecia Areata
Author(s):
At the 2022 Fall Clinical Dermatology Conference, 3 expert clinicians share their strategies for diagnosing and managing alopecia areata.
During an afternoon session at the 2022 Fall Clinical Dermatology Conference in Las Vegas, Nevada, Brett King, MD, PhD, associate professor of dermatology at the Yale School of Medicine, Valerie D. Callender, MD, founder and medical director of the Callender Dermatology & Cosmetic Center, and Maria K. Hordinsky, MD, professor and chair of the department of dermatology at the University of Minnesota, presented their strategies on diagnosing patients with alopecia areata (AA) and how to incorporate novel therapies into clinical practice.
AA is an autoimmune condition characterized by a rapid onset hair loss on the scalp, eyebrows, eyelashes, and in some severe cases, body involvement. AA can come with an unpredictable prognosis, with relapses, remissions, and persistent hair loss. Typically, AA is more prevalent in children, but it affects both sexes and all ethnicities equally.
Clinical presentations of AA include:
- Patchy hair loss
- Alopecia totalis
- Alopecia universalis
- Ophiasis pattern
- Inverse-Ophiasis (or sisaipho) pattern
- Diffuse pattern
- Alopecia barbae
- Alopecia areata of the nails
To accurately diagnose AA, dermatologists should complete a medical history review, physical exam, dermoscopy, hair pull test, and a biopsy. Another tool to use is the Alopecia Areta Investigator Globa Assessment (AA-IGA), which examines disease severity by the amount of scalp hair loss.
According to the speakers, there are multiple factors to consider when choosing a treatment option for children and adults with AA, such as:
- Age of the patient
- Location of the hair loss
- Disease extent
- Disease severity
- Presence of other medical conditions
- Scalp biopsy report on the hair cycle and inflammation
- Patient/parent choice after a thorough review of the proposed treatment and its risk, benefits, and expectations
For patchy AA, suggested treatments are topical or intralesional corticosteroids, minoxidil solution, anthralin, steroids in shampoo formulations, and topical immunotherapy. Treatment options for extensive AA include topical corticosteroids, topical minoxidil, topical immunotherapy, dithranol, oral vitamin D, phototherapy, laser therapy, and biologics.
Janus Kinase (JAK) inhibitors also show positive results for effectively managing AA. Oral ruxolitnib has been shown to induce hair regrowth in patients with moderate-to-severe AA. Tofacitinib is another JAK inhibitor that has been studied in relation to AA treatment for adolescents and adults.
To conclude their presentation, King, Callender, and Hordinsky stressed that there are various clinical presentations of AA ranging from patchy areas of hair loss to complete scalp involvement and body hair loss. Current treatments include topical, intralesional, and systemic interventions. However, these treatments demonstrate varying degrees of success.
Reference
King B, Callender V, Hordinsky M. The ‘how-to’ on diagnosing and managing alopecia areata. 2022 Fall Clinical Dermatology Conference. October 21, 2022. Las Vegas, Nevada.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.