- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Immunotherapies for Staphylococcus aureus
Author(s):
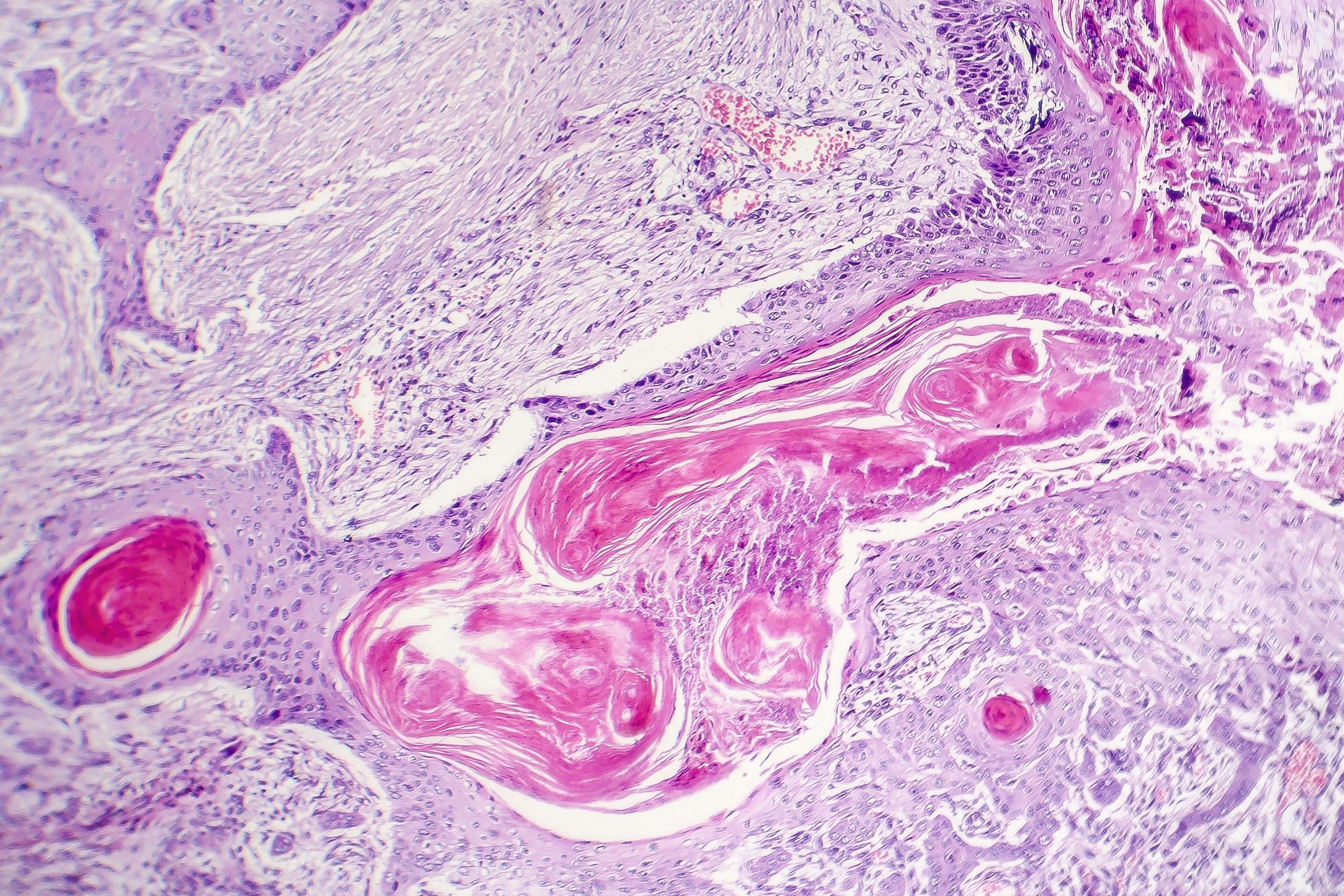
Staphylococcus aureus infections are becoming more challenging to treat due to methicillin-resistant Staphylococcus aureus (MRSA). A better understanding of cutaneous immune mechanisms will identify specific immune mechanisms to target for future vaccines and immunotherapies to ultimately address this serious public health threat.
“If immune-based therapies are to be an alternative to antibiotics then a greater understanding of the protective immune mechanisms and responses against Staphylococcus aureus skin infections is essential...,” says Lloyd S. Miller, M.D. (hereswendy - stock.adobe.com)

Lloyd S. Miller, M.D.
One of the most common human bacterial skin pathogens, Staphylococcus aureus, has become a major public health threat because of the widespread emergence of virulent community-acquired methicillin-resistant Staphylococcus aureus (MRSA) strains caused in part by overuse of antibiotics. One of the central goals of current research and development in immunotherapy is to fulfill an unmet need for therapeutic options that could help minimize the use of antibiotics while exhibiting efficacy against Staphylococcus aureus.
“If immune-based therapies are to be an alternative to antibiotics then a greater understanding of the protective immune mechanisms and responses against Staphylococcus aureus skin infections is essential so that we can engage the own host’s own immune system to help combat these infections. Our long-term goal is to uncover the mechanisms that serve as targets for immune-based therapies and vaccination strategies,” said Lloyd S. Miller, M.D., Ph.D., vice chair for research of dermatology and associate professor of dermatology, infectious diseases, orthopaedic surgery & materials science and Eengineering, Johns Hopkins Department of Dermatology, Baltimore, MD.
Previous research, including active (StaphVax®, Nabi Biopharmaceuticals and V710®, Merck, Inc.) and passive (Veronate®, Inhibitex, Inc.) vaccines targeting capsular polysaccharides, iron surface determinant B or clumping factor A on the surface of Staphylococcus aureus have all failed in clinical trials. According to Dr. Miller, potential effective treatment strategies against Staphylococcus aureus are now being directed towards an immune response mediated by T cells or T lymphocytes, which may contribute to more durable immune protection against these increasingly challenging to treat infections in the long term.
There are different types of T cell responses depending on the subset of T cells Dr. Miller said, including T effector cells that produce cytokines such as interleukin-17 (IL-17), tumor necrosis factor (TNF), and interferon gamma (IFNγ). These cytokines appear to engage the host’s neutrophil response, which involves the recruitment of neutrophils from the bloodstream to an abscess around the bacteria to help wall-off and clear the infection.
“In all of our models without these T cells, we do not see efficient and effective abscess formation, implicating the critical importance of the T cell responses. If we can learn the mechanisms to engage a memory T cell response against Staphylococcus aureus skin infections, it might be possible for the host immune system to clear these infections,” Dr. Miller said.
The research of the specific immune responses with T cells that can be targeted to promote immune clearance of Staphylococcus aureus is ongoing, the results of which will hopefully soon translate to the clinic. According to Dr. Miller, the focus is to promote specific T cell immune responses directed against the bacteria instead of leading to nonspecific immune activation.
“Ideally, the immune system and the specific T cell responses would have to be directed against the bacteria rather than something that could cross-react with the host and lead to unwanted and aberrant inflammatory and autoimmune diseases,” Dr. Miller said.
It is critically important to understand the actual immune correlates that lead to protection against Staphylococcus aureus infections. This is likely the reason why most of the vaccines have failed in human trials Dr. Miller said.
“I think if we learn more about the immune responses and really understand which mechanisms are mediating durable memory protection against the infection, we would be able to better target those immune responses for effective host immune clearance. I believe it that understanding these immune mechanisms is crucial to the future development of effective immunotherapies and vaccines,” Dr. Miller said.
Disclosures:
Boehringer Ingelheim – I(Grants/Research Funding); Medimmune – I(Grants/Research Funding); Moderna Therapeutics – I(Grants/Research Funding); Noveome Biotherapeutics – SH(ST); Pfizer Inc. – I(Grants/Research Funding); Regeneron – I(Grants/Research Funding);

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.