- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Managing Keloids and Hypertrophic Scars
Author(s):
Scarring is an essential part of the wound-healing process. Sometimes, when the healing process is disrupted, abnormalities in natural scarring occur that may lead to either a hypertrophic scar (HTS) or a keloid.1 HTS and keloids, mainly affecting younger populations aged 11 to 30 years, are formed when the balance between collagen synthesis and breakdown during scar maturation is lost, resulting in collagen accumulation, leaving a scar raised above the normal skin.1,2
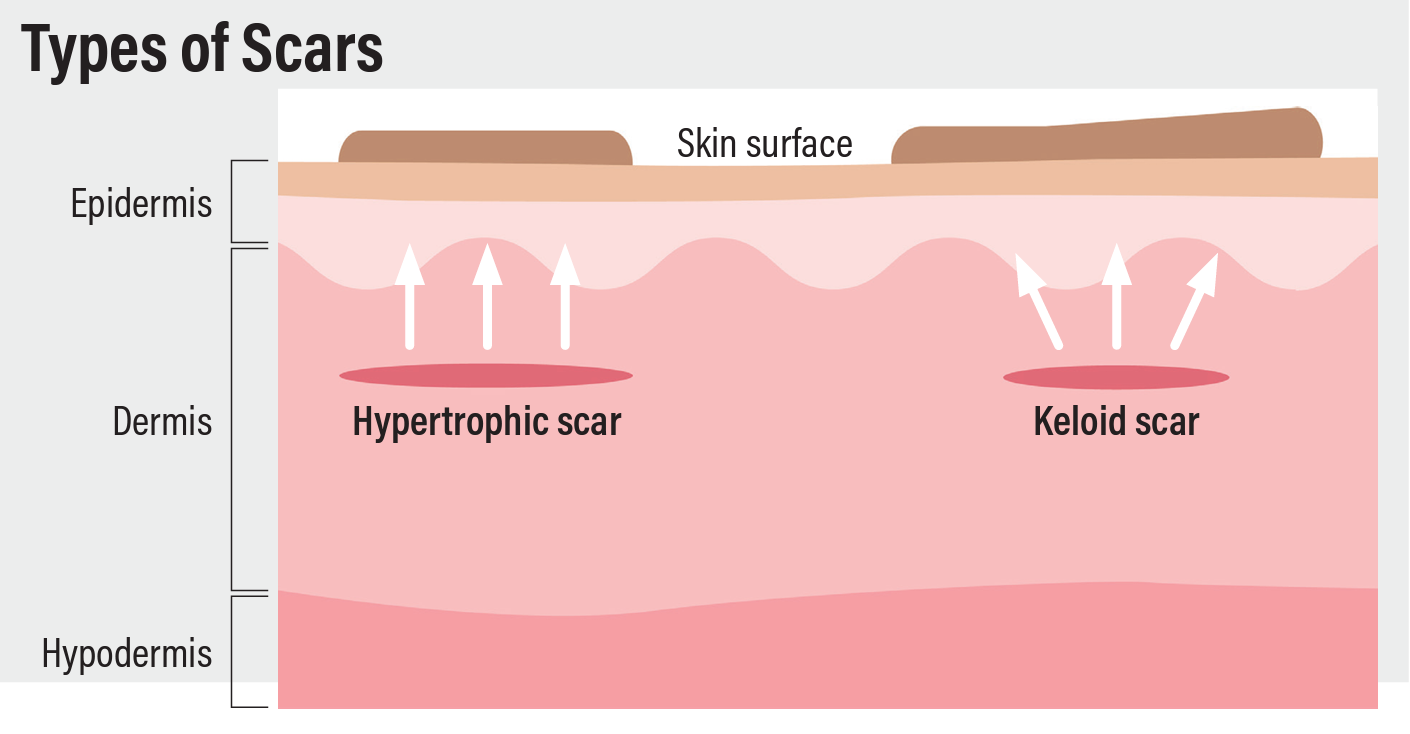
Although both of these are firm raised scars that can be asymptomatic, pruritic, or painful, and may even cause restrictions in movement, they primarily differ in that HTS remains within the site of the injury and may regress over time. In contrast, keloids are more severe, do not regress over time, and may extend beyond the site of the injury, with a tendency to recur. HTS usually appears on areas of high tension such as extensor joints, whereas keloids mostly appear on shoulders, earlobes, posterior neck, and upper back.3
Causes and Epidemiology
These scars are mainly caused by injuries deep enough to affect the reticular layer of the dermis. These injuries may be caused by burns, insect bites, surgery, tattoos, and piercings. Although the exact mechanism is still unknown, several associations have been linked to the formation of these unsightly scars. Studies have linked systemic inflammation and conditions increasing systemic inflammatory markers with increased risks of HTS and keloids. However, some studies have also reported increases in the incidence and size of keloids in patients who are hypertensive. Moreover, mechanical stresses on the wound also play an essential role in increasing the risk of HTS and keloids.2
Unlike HTS, keloid formation has a genetic predisposition, as they frequently appear in individuals with Fitzpatrick skin types IV to VI. Keloids are most prevalent in African American patients, followed by those who are Asian, Hispanic, and White.
Treatment Options
Various invasive and noninvasive treatment options exist for managing these scars. However, no 1 treatment is effective for all individuals. The treatment decision is mainly based on factors that include the site of the lesion, associated symptoms, distress caused to the patient, and severity of functional impairment caused by the lesion. Scars that are less than 1 year old and HTS, which regress over time, usually go away on their own and do not require treatment.1
Silicone Products
Silicone-based products are first-line noninvasive treatment options that are effective in reducing scar thickness, elasticity, and erythema. For optimal results, it is recommended to apply/wear the silicone gel/sheeting for a minimum of 12 hours daily for 6 to 12 months.1
Intralesional Corticosteroids
In case of severe pruritic scars where silicone products are ineffective, intralesional steroid injections may help manage the scars. Intralesional corticosteroids, such as triamcinolone, have long been considered a first-line treatment regimen for keloids and HTS.1 Corticosteroids act by inhibiting collagen and glycosaminoglycan production and by reducing fibroblast proliferation while breaking the existing ones. However, triamcinolone induces collagenase production and decreases the level of collagenase inhibitors, thereby degenerating collagen nodules, which is a characteristic feature of keloids.
Adverse effects of intralesional corticosteroids may include dermal thinning, fat atrophy, and pigment changes. Other corticosteroids that may help improve the appearance of these scars include dexamethasone, hydrocortisone acetate, and methylprednisolone.3
Receptor Blockers
Angiotensin II type 1 and type 2 receptors are upregulated in human skin wounds. Angiotensin II type 1 receptor signaling increases collagen production and angiogenesis, whereas angiotensin II receptor blockers inhibit these pathways.4 Several studies have demonstrated the efficacy of losartan ointment against keloids and HTS. Moreover, similar benefits have been seen with the use of angiotensin-converting enzyme inhibitors, including ramipril, captopril, and enalapril, in the management of keloids and HTS, specifically from burns.1
Dupilumab
The use of dupilumab (Dupixent) has been gaining traction among dermatologists in the treatment of HTS and keloids. Dupilumab is a monoclonal antibody that blocks IL-4 and IL-13 signaling, thereby reducing abnormal scarring. Studies have shown that after being treated with dupilumab, patients experience shrinkage of large keloids and disappearance of smaller ones.1
Bleomycin
Intralesional injections of bleomycin, a glycopeptide antibiotic that possesess antitumor, antibacterial, and antiviral activity, have been effective in treating keloids and HTS. A comparative study published in the Journal of Dermatology & Dermatologic Surgery found intralesional bleomycin injections to be more effective than 5-fluorouracil (5-FU) alone or 5-FU combined with triamcinolone, with a lower risk of relapse.5
Cryotherapy
Intralesional cryotherapy is a relatively new development that uses a double lumen needle placed through the core of a keloid or HTS and delivers nitrogen vapor, freezing the scar from its core, outward.6 Despite limited data, some studies suggest cryotherapy as a safe adjunct treatment option for optimal scar reduction in a few treatment cycles. Adverse effects are uncommon but may include depigmentation, pain, and recurrence.1
Pentoxifylline
Oral pentoxifylline, a methylxanthine derivative, has been shown to be effective in the treatment of keloids. A study published in Dermatologic Surgery found that high-risk patients who took 400 mg of oral pentoxifylline 3 times a day for 6 months after surgical excision of a keloid had a lower risk of recurrence than patients who didn’t take pentoxifylline postsurgically.7 Another study compared intralesional injections of pentoxifylline and triamcinolone and found pentoxifylline to be safer and better tolerated than triamcinolone but less effective when used alone. Hence, it is suggested to use them in combination for improved results and to lower the risks of steroid-associated adverse effects.8
5-FU
5-FU, a pyrimidine analogue, is an effective and painless treatment option for both keloids and HTS.3 It works by inhibiting fibroblast proliferation, inducing apoptosis without necrosis, and inhibiting the synthesis of TGF-β–induced type I collagen. Although injections of 5-FU alone may significantly improve keloid appearance, it is more effective in reducing the scar size than laser, topical, and physical treatments when combined with triamcinolone.1
Laser Therapy
Laser treatment is a relatively new development in the management of keloids and HTS. Because laser therapy is expensive and has adverse effects, it is considered a second-line or third-line treatment option for managing HTS and keloids. A systemic review found fractional ablative carbon dioxide lasers (10,600 nm) and erbium-doped yttrium aluminum garnet lasers (2940 nm) to be slightly more effective in reducing the height, erythema, and pliability of the scars than pulsed dye lasers (585 nm).9
Surgical Excision
Surgical excision is the standard treatment of keloids and is often required in refractory cases. However, it may stimulate collagen synthesis, so the chances of recurrence are high. To prevent additional collagen synthesis, intramarginal excision of keloids is recommended.10
This can be used alone but sometimes requires the application of adjuvant treatments such as radiation or topical therapy. Approximately 50% to 80% of cases recur after being treated with surgery alone. However, the use of corticosteroids lowers the recurrent rate to less than 50%, which further reduces to less than 10% with the help of radiotherapy and produces the best results when administered within 2 days of surgery at a dose of 30 Gy.1
Noninvasive Treatment
Although there are limited data, studies support the use of compression therapy 23 hours a day at 20 to 40 mm Hg of pressure to reduce scar thickness and hardness. Onion extract gel is another noninvasive adjunctive treatment option that may help improve redness, softness, and overall texture at the excision site after superficial shaving of the skin lesion; however, it is ineffective in treating deep scars. Moreover, evidence suggests that triamcinolone combined with onion extract is more effective in relieving pain and itching than triamcinolone alone.1
Prevention
To prevent the formation of these scars, it is recommended to avoid causing nonessential trauma to the skin, such as piercing or cosmetic surgery. Postsurgical scarring can be reduced with careful planning, as incisions made parallel to the Langer lines heal with better outcomes than incisions that cut across those lines.
Given that HTS and keloids result from chronic inflammation in the reticular dermis, certain surgical techniques such as hiding sutures in natural skin folds and limiting the wound to a single cosmetic subunit may reduce tension on the edges of the wound, thereby preventing scar formation.1 Moreover, subcutaneous/fascial tensile reduction sutures for wound closure significantly reduce the risk of scar formation.11
Several studies have reported postsurgical treatment with silicone gel effectively prevents and improves the appearance of HTS and keloid formation. By hydrating the stratum corneum, silicone gel reduces collagen production, thereby encouraging the normal healing process. Additionally, a study published in Plastic and Reconstructive Surgery found that the use of paper tape for 12 weeks significantly reduced HTS formation and decreased the volume of scars that had already formed12; however, there are little data available on the efficacy of paper tape in preventing HTS formation.
References
- Kim EY, Hussain A, Khachemoune A. Evidence-based management of keloids and hypertrophic scars in dermatology. Arch Dermatol Res. Published online December 11, 2022. doi:10.1007/s00403-022-02509-x
- Carswell L, Borger J. Hypertrophic scarring keloids. In: StatPearls. Treasure Island (FL): StatPearls Publishing; March 11, 2023.
- Tripathi S, Soni K, Agrawal P, Gour V, Mondal R, Soni V. Hypertrophic scars and keloids: a review and current treatment modalities. Biomed Dermatol. 2020;4(11). doi:10.1186/s41702-020-00063-8
- Niazi F, Hooshyar SH, Hedayatyanfard K, et al. Detection of angiotensin II and AT1 receptor concentrations in keloid and hypertrophic scar. J Clin Aesthet Dermatol. 2018;11(10):36-39.
- Kabel AM, Sabry HH, Sorour NE, Moharm FM. Comparative study between intralesional injection of bleomycin and 5-fluorouracil in the treatment of keloids and hypertrophic scars. J Dermatol. 2016;20(1):32-38. doi:10.1016/j.jdds.2015.07.003
- O’Boyle CP, Shayan-Arani H, Hamada MW. Intralesional cryotherapy for hypertrophic scars and keloids: a review. Scars Burn Heal. 2017;3:2059513117702162. doi:10.1177/2059513117702162
- Tan A, Martinez Luna O, Glass DA 2nd. Pentoxifylline for the prevention of postsurgical keloid recurrence. Dermatol Surg. 2020;46(10):1353-1356. doi:10.1097/DSS.0000000000002090
- Serag-Eldin YMA, Mahmoud WH, Gamea MM, Hegab DS. Intralesional pentoxifylline, triamcinolone acetonide, and their combination for treatment of keloid scars. J Cosmet Dermatol. 2021;20(10):3330-3340. doi:10.1111/jocd.14305
- Oosterhoff TCH, Beekman VK, van der List JP, Niessen FB. Laser treatment of specific scar characteristics in hypertrophic scars and keloid: a systematic review. J Plast Reconstr Aesthet Surg. 2021;74(1):48-64. doi:10.1016/j.bjps.2020.08.108
- Lemperle G, Schierle J, Kitoga KE, Kassem-Trautmann K, Sachs C, Dimmler A. Keloids: which types can be excised without risk of recurrence? A new clinical classification. Plast Reconstr Surg Glob Open. 2020;8(3):e2582. doi:10.1097/GOX.0000000000002582
- Ogawa R. Ideal wound closure methods for minimizing scarring after surgery. In: Téot L, Mustoe TA, Middelkoop E, Gauglitz GG, eds. Textbook on Scar Management. Springer Cham; 2020:185-191.
- Atkinson JA, McKenna KT, Barnett AG, McGrath DJ, Rudd M. A randomized, controlled trial to determine the efficacy of paper tape in preventing hypertrophic scar formation in surgical incisions that traverse Langer’s skin tension lines. Plast Reconstr Surg. 2005;116(6):1648-1658. doi:10.1097/01.prs.0000187147.73963.a5

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.