- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Misinformation delays rosacea diagnosis in skin of color patients
Author(s):
The idea that rosacea is uncommon in darker skinned individuals may be due to under-recognition. Careful clinical examination, a thorough history and biopsy in some cases are needed for accurate diagnosis and differentiating rosacea from diseases that may be more common.
Rosacea occurs across the entire spectrum of skin of color patients. Knowledge about its epidemiology is the foundation for early recognition and safe, effective treatment, says Theodore Rosen, M.D., who spoke during the Skin of Color Update virtual meeting September 12-13.
“According to some older publications, rosacea is not even seen among individuals with skin of color. Such misinformation can lead to a delay in diagnosis,” says Dr. Rosen, professor of dermatology, Baylor College of Medicine, Houston. “Maintaining an index of suspicion for rosacea and including it in the differential diagnosis is the first step to timely identification.”
Prevalence Data
According to a 2018 meta-analysis, rosacea had an estimated global prevalence of 5.5% among adults. Information on prevalence among U.S. patients with skin of color is available from a study examining data from the U.S. National Ambulatory Medical Care Survey for the years 1993 to 2010. Of the approximately 31.5 million rosacea visits included, approximately 2% were for black patients, approximately 2% were for Asians, and Hispanic or Latino patients accounted for approximately 4% of the visits.
“Added together, those rates suggest a prevalence of about 8% among skin of color patients, indicating that rosacea is certainly not unheard of in this group. In addition, keep in mind, that the skin of color population also includes people of Mediterranean and Middle Eastern descent and representing multiple Asian countries. Individual studies report rosacea among skin of color patients residing in a range of global regions,” Dr. Rosen says.
Clinical Findings
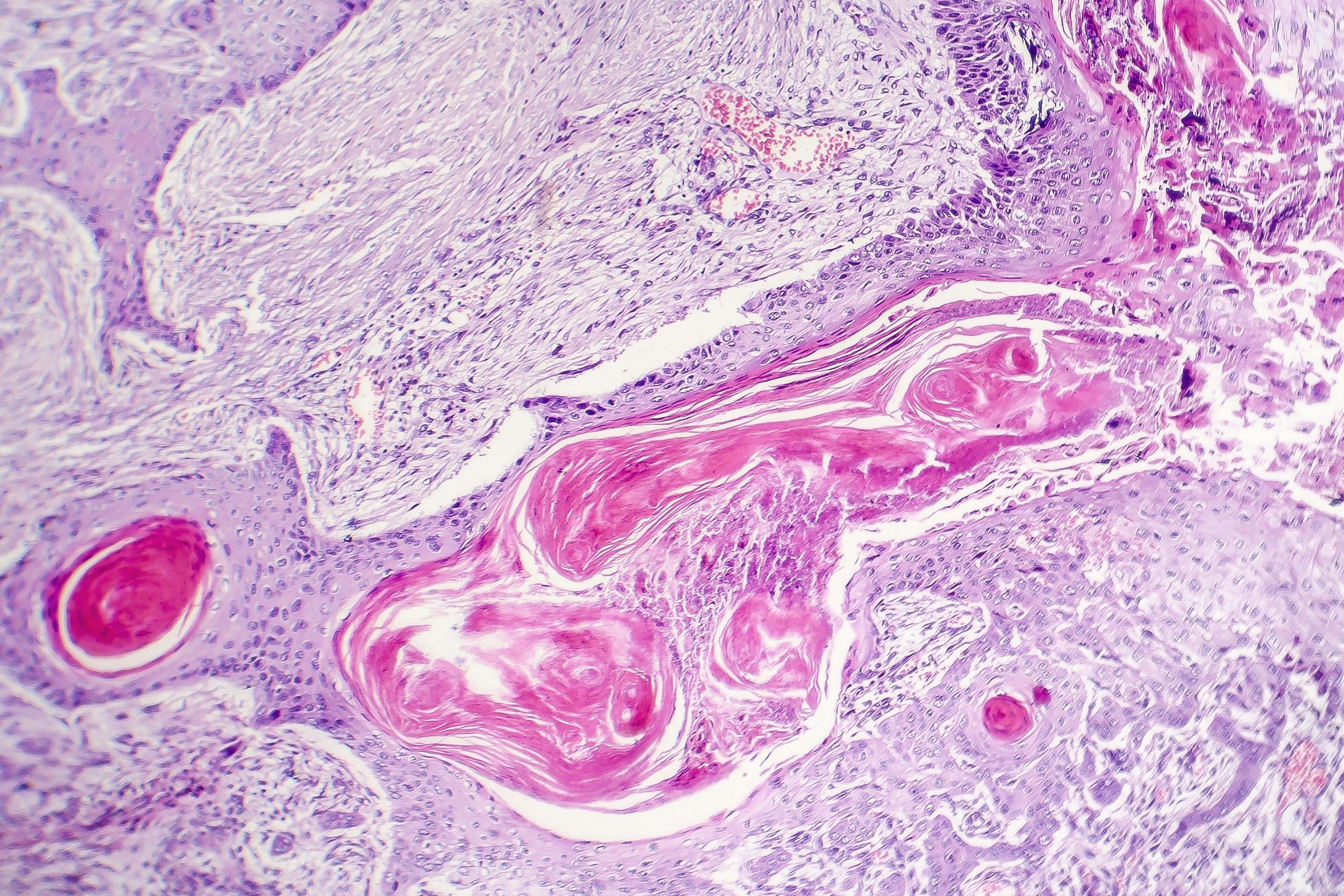
Difficulty recognizing some of the manifestations of rosacea in darker skinned patients may contribute to its under-diagnosis. However, all of rosacea's features (i.e., fixed centrofacial erythema, phymatous changes, flushing, papules and pustules, telangiectasia, and ocular manifestations) have been described in patients with skin of color. Rosacea in black patients may also be associated with granulomatous lesions. Dr. Rosen notes that, in particular, erythema and telangiectasias may be more difficult to detect in people with darker skin.
Because rosacea might be considered rare or non-existent in skin of color, the diagnosis may be overlooked for other diseases that are more prevalent. For example, African Americans may be misdiagnosed with systemic lupus erythematosus, dermatomyositis, or sarcoidosis, and acne vulgaris may be misdiagnosed across the spectrum of skin of color patients who present with papules and pustules.
“Careful examination and thorough history will help lead to the correct diagnosis,” Dr. Rosen says. “In most cases of rosacea, there is an initial history of excessive flushing whereas the other diseases are unlikely to be associated with flushing.”
Patient age may provide another clue for differentiating acne vulgaris and rosacea because rosacea tends to occur in older individuals, although there is overlap in the age range of patients affected by the two diseases. Additional signs for establishing a diagnosis of rosacea include a history of flushing and absence of comedonal lesions.
Dr. Rosen says that the granulomatous form of rosacea in black patients may be difficult to distinguish from sarcoidosis based on clinical appearance alone. With rosacea, however, patients tend to present with nodules located primarily around the eyes and nose, and notably patients with the granulomatous variant of rosacea are not affected by flushing and persistent erythema.
“Biopsy for histopathological examination should be considered for an accurate diagnosis,” Dr. Rosen says.
Treatment Approach
Medical approaches used to treat rosacea are the same for fair-skinned patients and those within the skin of color population. Laser and light therapy are also part of the armamentarium for treating rosacea-associated telangiectasias, erythema, and phyma in skin of color patients, but with the caveat that care must be taken to use the proper setting that will minimize the risk of post-treatment pigmentary changes and scarring, Dr. Rosen says.
“Laser and light interventions need to be used very judiciously and perhaps are best done in the hands of dermatologists who have experience with these modalities in the skin of color population,” he states.
Awareness and control of trigger factors also are a component of rosacea management for skin of color patients.
“It is interesting that on a global basis, many skin of color populations live in hot, humid regions, so that rosacea in these individuals may be aggravated by the environmental conditions,” Dr. Rosen says.
He adds that there is no evidence of any ethnic/racial differences in therapeutic response to the various agents used for rosacea management, but more research may be needed.
“This topic remains an open question because rigorous head-to-head trials comparing different demographic groups have not been done,” he says. “Similarly, the prognosis of rosacea also seems to be the same in fair-skinned individuals and various skin of color subgroups, although there is also a lack of long-term study data for the skin of color population.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.