- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Nail Surgery Pearls With Jane Bellet, MD
Author(s):
The nail expert from Duke University shares surgical techniques from biopsy to post-operative care.
Jane Bellet, MD, FAAD
When course directors surveyed members of the Society of Pediatric Dermatology to determine sessions for this year's 48th annual meeting, an overwhelming number of pediatric dermatologists expressed the desire for additional nail knowledge. Jane Bellet, MD, FAAD, professor of pediatrics and dermatology at Duke University School of Medicine, presented nail surgery pearls during the session "Tiny Toes, Big Care: Navigating Pediatric Nail Procedures with Confidence" at the 2023 Society for Pediatric Dermatology Meeting in Asheville, North Carolina, July 13-16.1
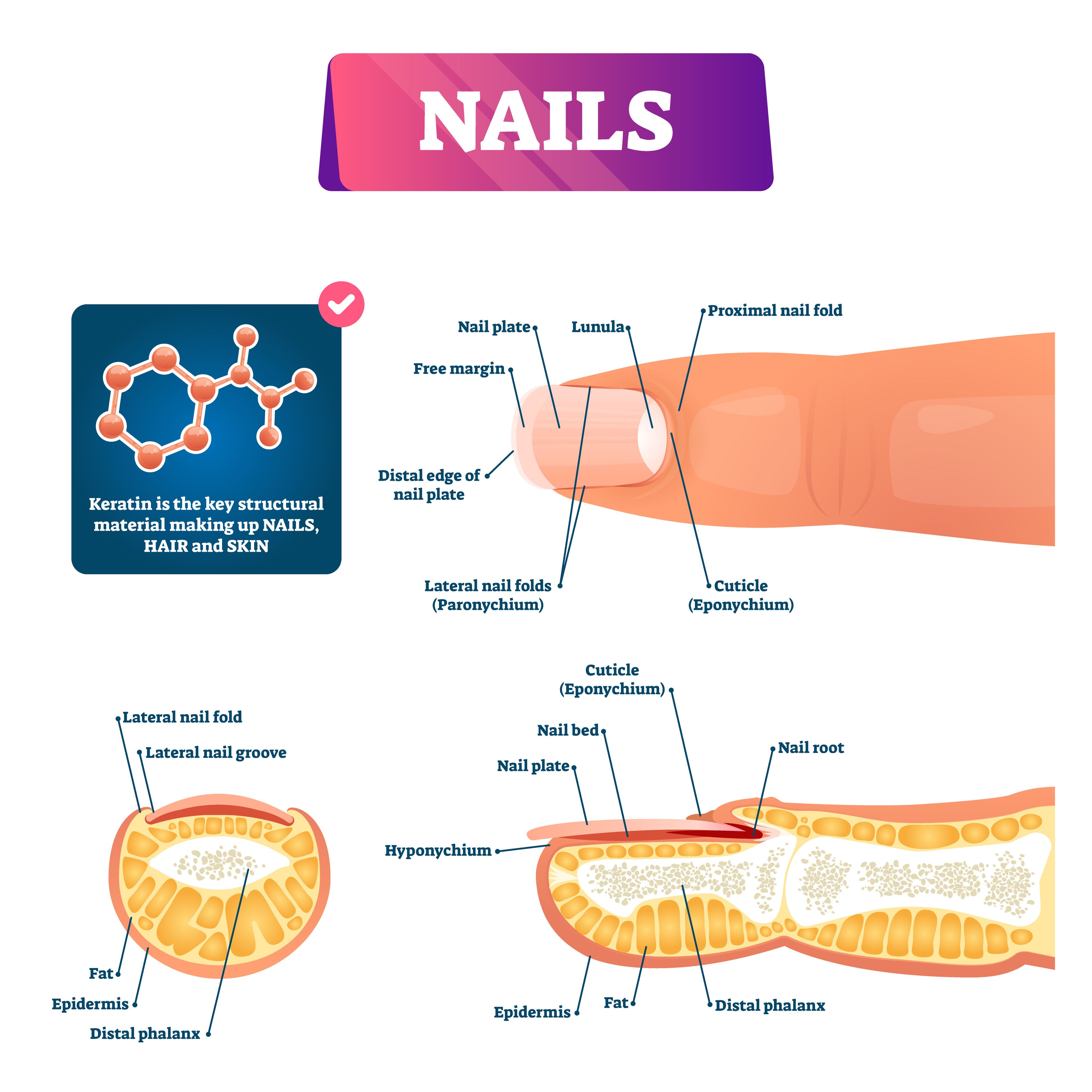
Bellet first pointed out the importance of knowing nail anatomy. The primary focuses are usually on the plate, eponychium, lanula, and hyponychium. "Every patient with nail pigmentation needs onychoscopy. Most patients do not need biopsy, but don't be afraid to biopsy if it will guide management, if you're worried, or if it's weird," she said.
Basic nail procedures include punch biopsy (<3 mm), nail avulsion (partial or full), matricectomy (chemical or physical). Advanced nail procedures include nail matrix shave excision, lateral longitudinal bed excision, and en bloc excision. Overall, the approach to nail surgery and care for pediatric adults is the same as adults, not necessarily more difficult.
To prepare for surgery, soak the hand or foot in warm water and chlorhexidine to soften the nail and make marks prior to administering anesthesia. Bellet uses local block anesthesia for all of her cases. General anesthesia is for <12 year olds because they must be able to stay still. For antisepsis, Bellet recommends an extensive surgical scrub of the entire hand or foot with chlorhexidine scrub brushes.
Nailing down a bloodless field with the right tourniquet presents a few techniques. A sterile glove can be used as part of the draping process. The penrose drain requires wrapping distal to proximal and secure with hemostat. Bellet is a personal fan of the T-ring tourniquet. Her surgical tools of choice include double action nail clippers, an English anvil-action nail splitter, and a nail elevator (spatula).
"If you remember 1 thing about this session, please remember that the physician should always take off the tourniquet," Bellet shared. "You can have the best team surrounding a surgery, but the consequences of not taking the tourniquet are too dire."
There are a few specific techniques Bellet reviewed to make certain procedures go more smoothly.
- In a partial proximal avulsion, an English anvil-action nail splitter will be needed. Transverse cut to the other lateral sulcus, reflect laterally, and secure with a hemostat before making 2-3 reflecting incisions.
- For a nail matrix shave, utilize a polymer coated 15 blade before scoring and cutting parallel to the epithelium.
- If you are working with the avulse 5th toenail, remove en bloc since the nail is so small.
- Onycocryptosis are often unilateral, but can be bilateral. It affects mechanics of the foot and nail and often stems from incorrect trimming or wearing shoes that are too tight. Management has a variety of approaches including disinfection 1-2 times a day, topical steroids, anchor taping, dental floss/cotton wick, systemic antibiotics (if there is infection), cotton cast with cyanoacrylate, chemical avulsion (urea 50% ointment under occlusion, ablation (phenol, TCA, sliver nitrate, electrocautery)
Bellet explained that bandaging after a nail producure should always be longitudinal with 2x2 gauze, matisol, tape, and stockinette. Monitor for at least 15 minutes to ensure bleeding stops and re-bandage if needed. For children who may run and jump after leaving the office, more padding and immobilization with splints, slings, or boots may be needed.
Post-operative care has special considerations with pediatric patients. It may be difficult for them to keep bandages on for a variety of reasons including requirements to wash hands at daycare or school, sports seasons, and toddlers tending to suck their fingers. Writing clear instructions for parents and guardians is key when it comes to pain management, leaving the bandage on for 48-72 hours, warm soaks, re-bandaging, and checkups 2-4 weeks later. Nail healing requires patience as it may take several months.
At the conclusion of her presentation, Bellet emphasized the importance of networking with local hand, plastic, and orthopedic surgeons and podiatrists.
Reference
1. Bellet J. Tiny toes, big care: navigating pediatric nail procedures with confidence. Presented at the 2023 Society for Pediatric Dermatology Meeting; July 13-16, 2023; Asheville, NC.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.