- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Article
Understanding psoriasis induced by TNF-a inhibition
Author(s):
Researchers at The Cleveland Clinic Lerner College of Medicine recently explored the development of a psoriasiform rash in patients with inflammatory bowel disease or rheumatoid arthritis who were treated with TNF-ɑ inhibitors. Learn what they discovered in this article.
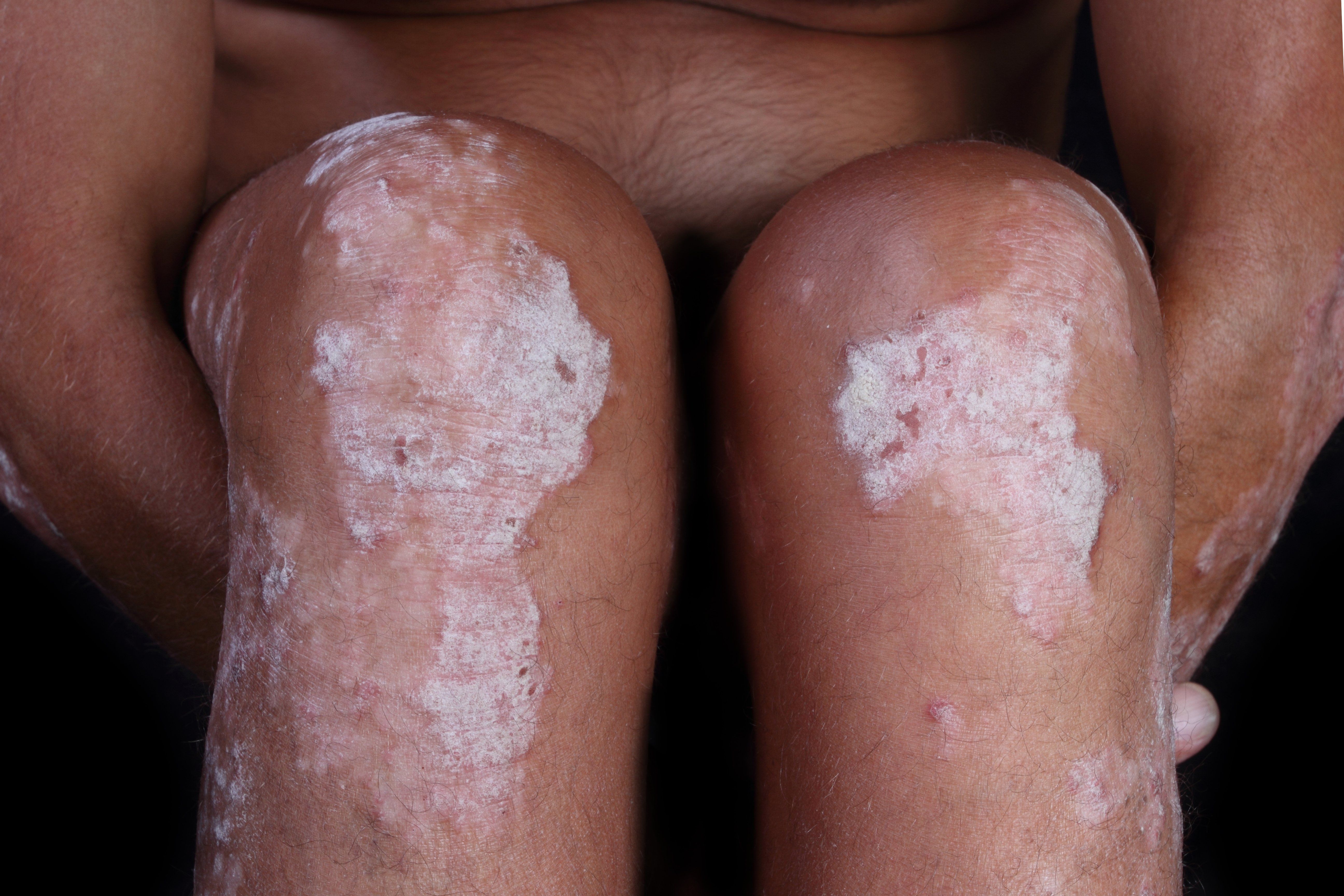
Researchers at The Cleveland Clinic Lerner College of Medicine recently explored the development of a psoriasiform rash in psoriasis patients treated with TNF-ɑ inhibitors. Learn what they discovered in this article. (Antonio Nardell - stock.adobe.com)
The treatment of psoriasis was revolutionized with the invention of biologics. Tumor necrosis factor alpha (TNF-É) inhibitors have played a prominent role in establishing effective biologic treatments in psoriasis. However, one of the paradoxical adverse reaction associated with this therapy is the development of a psoriasiform rash.
Dr. Fernandez and his fellow researchers at The Cleveland Clinic Lerner College of Medicine explored this phenomenon in greater detail. Their results were published in the Journal of American College of Dermatology in July of 2018.
They performed a retrospective study identifying all of the TNF-É inhibitor-associated psoriasis over a 10 year period at the Cleveland Clinic. Approximately one hundred cases of TNF-É inhibitor-associated psoriasis were discovered. The majority of the cases were female with a 2.6:1 ratio.
Most of the cases identified were receiving TNF-É inhibitors for inflammatory bowel disease and rheumatoid arthritis. Interestingly 14.4% of the patients that developed psoriasis while receiving anti-TNF-É therapy had a relative with psoriasis. In this retrospective review, the most common anti-TNF-É therapy associated with psoriasis was infliximab therapy followed by adalimumab.
Of the patients that developed a psoriasiform rash on anti-TNF-É therapy, 60% developed more than one psoriasis subtype. The most common subtype associated with anti-TNF-É therapy was plaque psoriasis followed by scalp psoriasis. Generalized pustular psoriasis was the least common, reported in only 3% of cases.
Using the same cohort the authors also reviewed the specific cases in order to describe the treatment provided for psoriasis associated with anti-TNF-É therapy. They discovered that in some patients topicals alone can induce resolution of rash, however, some cases require stopping the biologic treatment.
Dr. Fernandez et al created a algorithm based on their retrospective cohort to assist with management of psoriasis associated with anti-TNF-É therapy. In the algorithm patients with well-controlled disease on anti-TNF-É therapy with a mild psoriasiform eruption should receive topical therapy. If the rash persists they should receive DMARDs and phototherapy. If the rash remains their anti-TNF-É therapy should be changed to another class of anti-TNF-É therapy.
In a patient with well-controlled disease on anti-TNF-É therapy who develops a severe psoriasiform eruption, DMARDs and phototherapy should be added. If, however, the rash remains the class of anti-TNF-É therapy should be changed.
This study represents the largest single-institution cohort of patients with psoriasis induced by TNF-É therapy. Using the institution’s experience the authors also provide a framework to treat this form of psoriasis. However, given the limitation of this retrospective cohort additional studies are needed to better understand this phenomenon.
Reference:
Mazloom, Sean E., et al. "TNF-α Inhibitor-Induced psoriasis: A decade of experience at the Cleveland Clinic." Journal of the American Academy of Dermatology (2018).
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.







