- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Psychodermatology: Where the skin and mind meet
Author(s):
This article is the first of our series on psychodermatology from Gina M. Caputo, D.O. In it, she highlights the prevalence of emotional disorders in patients with skin diseases, and introduces the four main classifications of psychodermatological disorders.
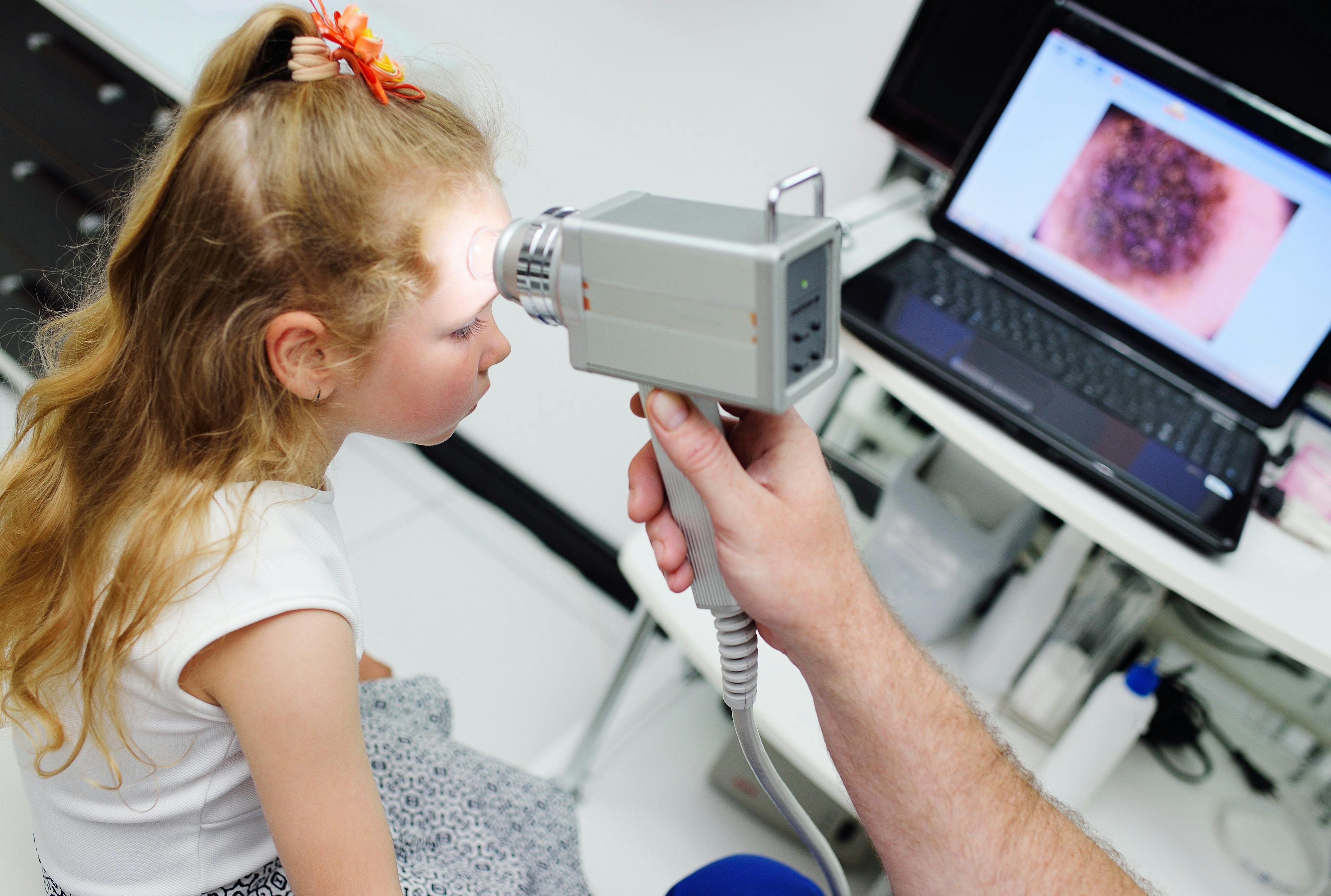
The understanding of the relationship between the psyche and the skin is complex, fascinating, and one that puzzles many physicians. (©Sfamphoto/Shutterstock.com)

Gina M. Caputo, D.O.

There are many fields of medicine that cross over into our specialty. As dermatologists, it is easy to co-manage and identify the psoriasis patient with psoriatic arthritis, the patient with alopecia receiving chemotherapy for her breast cancer, and the patient on dialysis with uremic pruritus. Conversely, the patient with the bugs crawling under his skin, the itchy elderly widower, and the depressed acne patient become more of a challenge.
One-third of all patients in dermatology have emotional disorders.1 The understanding of the relationship between the psyche and the skin is complex, fascinating, and one that puzzles many physicians.
Many of the chief complaints brought to dermatologists have a psychosocial issue associated with it. Psychodermatology/ psychocutaneous medicine encompasses many different types of conditions that are both psychiatric and dermatologic. It is crucial that dermatologists identify these overlapping situations because psychodermatological patients often refuse a psychiatry referral. In fact, often times recommending a referral before trust is formed, can make the patient feel isolated and make the condition worse.
Psychodermatological disorders can be classified into four different categories: Psychophysiological disorders, primary psychiatric disorders, secondary psychiatric disorders, and cutaneous sensory disorders.
Psychophysiological disorders are true dermatologic diseases that are exacerbated by emotional stressors. Conditions like atopic dermatitis, acne, perioral dermatitis, psoriasis, and hyperhidrosis are all examples of conditions that patients often report worsen when they are under stress. When a patient presents with a flare, it is not uncommon that, when prompted, the patient will report some stressor in his everyday life.
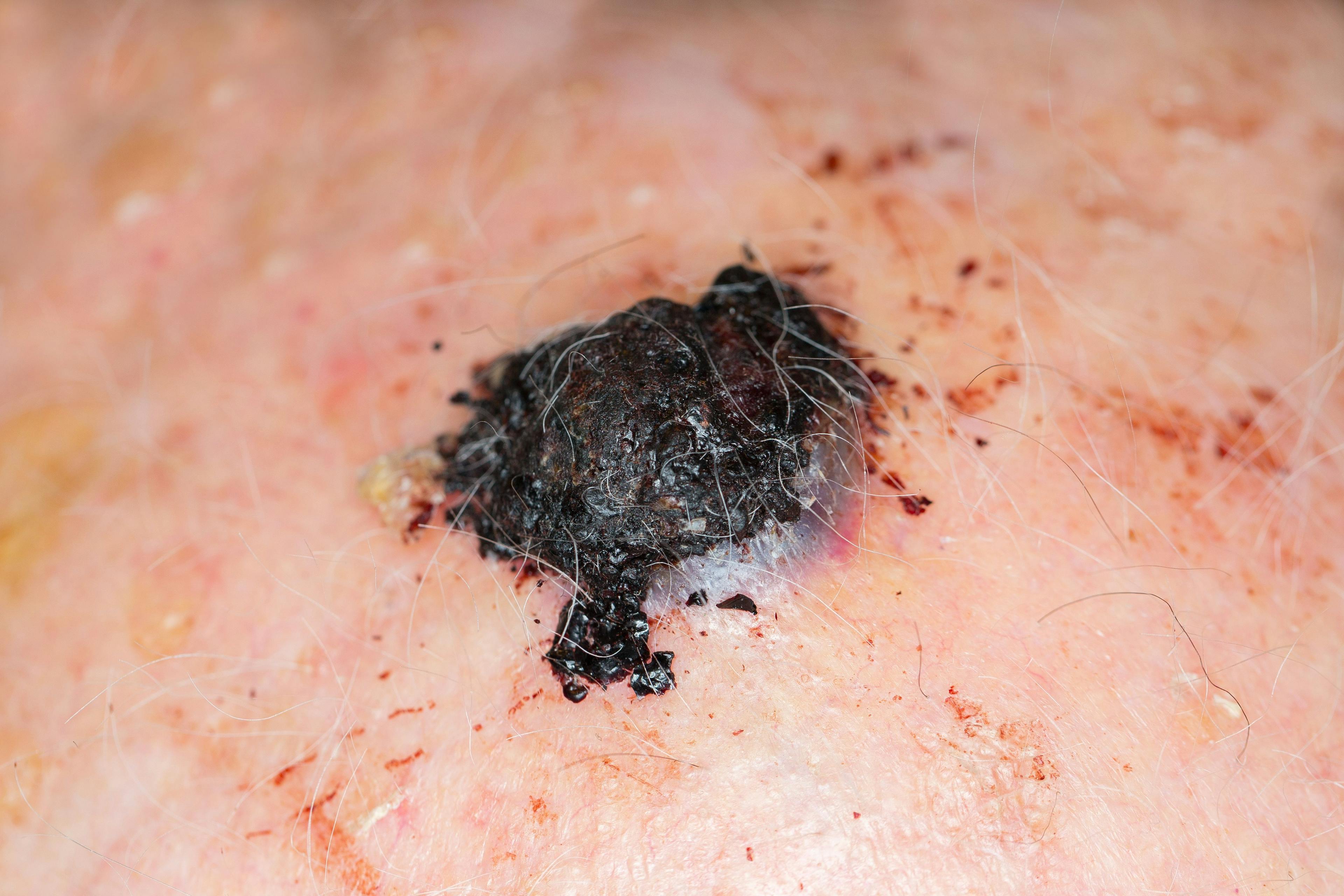
Primary psychiatric disorders, on the other hand, have no real skin disease, but, instead, have serious psychopathy. The classic examples of these conditions are delusions of parasitosis, dermatitis artefacta, and trichotillomania. These patients often present after seeing multiple doctors and have bizarre atypical skin lesions, stories, beliefs and samples for examination.
Secondary psychiatric disorders describe psychological disorders that patients develop in response to their dermatologic disease. Vitiligo, acne, alopecia areata, hidradenitis suppurativa, and psoriasis are all dermatologic conditions that can have a significant impact on the emotional health and well-being of a patient. Due to the severity or believed severity of their disease, many patients develop psychological distress. Cutaneous sensory disorders are akin to chronic pain syndrome. These disorders are the dysethesias and unpleasant sensations of biting, stinging, burning, and itching without any clear etiology.
Cutaneous sensory disorders often times may present with or without psychiatric disturbances, but depression and anxiety are the most common comorbid conditions.2
There is an enormous amount of pressure put on a dermatologist when patients present to our offices, especially when they have been seen by six other physicians for their complaint. We are often a patient’s last hope. If, after multiple visits, an organic cause has not yet presented itself, it is important that we take the time to shake out the details as to what is the underlying cause of their complaint.
It can be hard to use your “third eye” for these cases when you are 45 minutes behind and there are six drug reps in the hallway harassing you. Patients simply want to be heard and have their feelings validated. Acknowledging an acne patient’s frustrations, asking a psoriasis patient how they are emotionally dealing with their disease, or simply pausing to acknowledge a patient’s struggles, can help to foster a trusting, safe environment that will allow the physician to ultimately identify the issue and work towards fixing it.
In this upcoming series, my objective is to dive into the different categories of psychodermatological diseases, and discuss how to recognize, address and co-manage each of the different entities. Â
References:
1. Harth W, Gieler U, Kusnir D, Tausk FA. Clinical Management in Psychodermatology. 1st ed. Berlin, Heidelberg: Springer; 2010.
2. Koo J, Lee CS. Psychocutaneous Medicine. New York: Marcel Dekker, Inc; 2003.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.