- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Can treating warts do more harm than good?
Author(s):
When it comes to easily-recognized, benign, self-limited conditions like warts and molluscum, Dr. Siegfried calls herself a treatment nihilist. Learn why in this article.
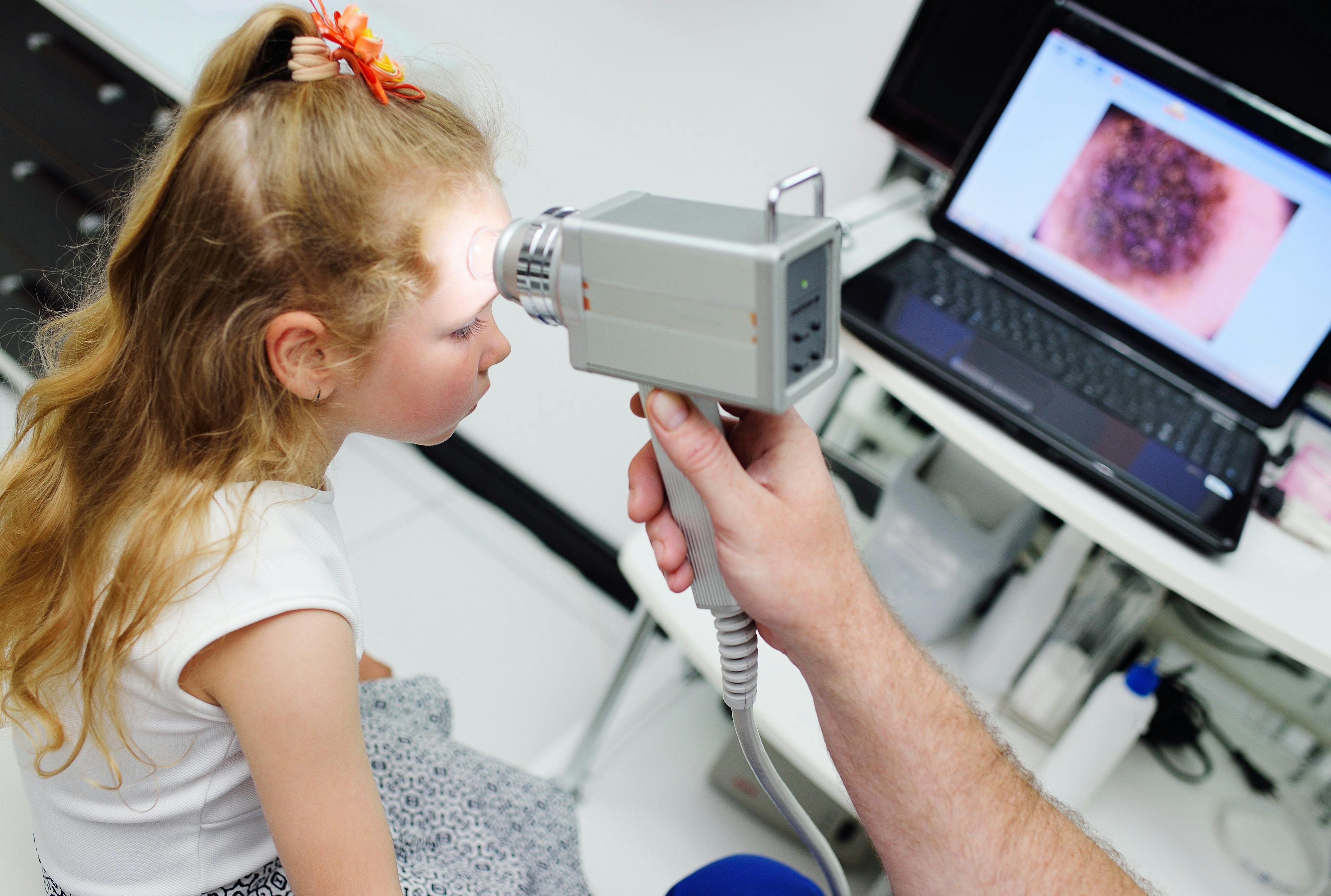
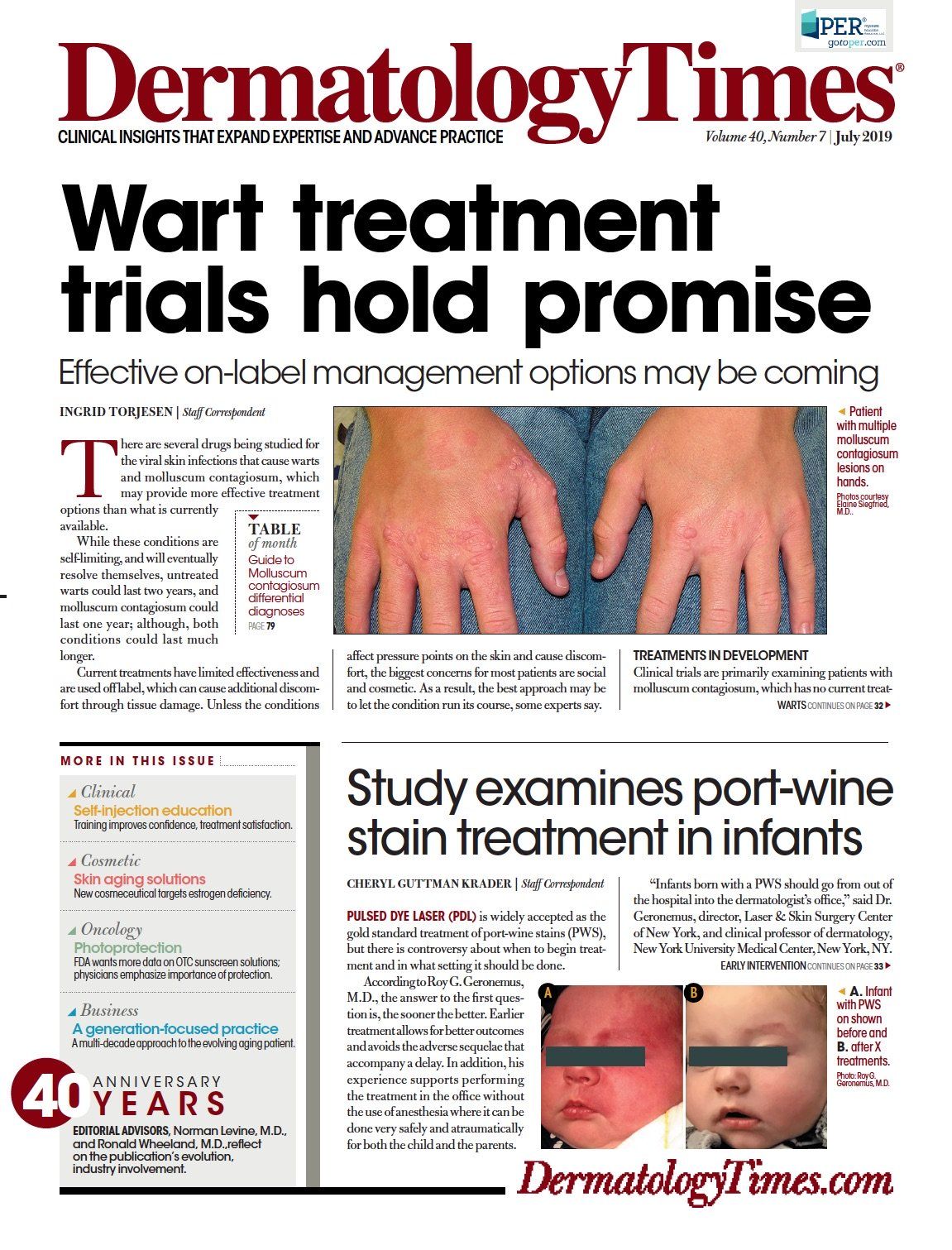
Many patients expect a treatment and are dissatisfied with mere anticipatory guidance about the natural history, iatrogenic risks and lack of a uniformly effective best option. (©MarcelJanovic/Shutterstock.com)

Dr. Siegfried

Warts and molluscum are common, benign and self-limited conditions that are considered much more than a nuisance for the many patients (and parents of pediatric patients) who visit a dermatologist. There is a long list of potential treatments for these conditions because the number of options is often inversely proportional to the efficacy of the best one.
Many patients expect a treatment and are dissatisfied with mere anticipatory guidance about the natural history, iatrogenic risks and lack of a uniformly effective best option. Dermatologists often feel obliged to do something and usually resort to liquid nitrogen cryotherapy, the most efficient in-office treatment, and one which has a defined procedure code. But this approach only satisfies one of the timeless criteria for practicing the art of medicine: “to cure sometimes, to relieve often, to comfort always.”1
As healers, our quest to cure can overshadow the fundamental principle of bioethics, “primum non nocere.” Striving to solve problems can also create them. Most interventions have risks and unintended consequences that must be weighed carefully against the risk of the disease. Medical or surgical intervention is not always the best solution for a perceived problem, and every problem is not as easily addressed as a nail that can be driven with a hammer. So, one of my mottos is: never recommend evaluation OR treatment with higher risks than the worst possible diagnosis in the differential.
When it comes to easily recognized, benign, self-limited conditions, I have increasingly become a treatment nihilist. This bias is the cumulative result of many memorable patients I have seen in the last 30 years who received treatments with associated risks that far outweighed those of their skin disease.
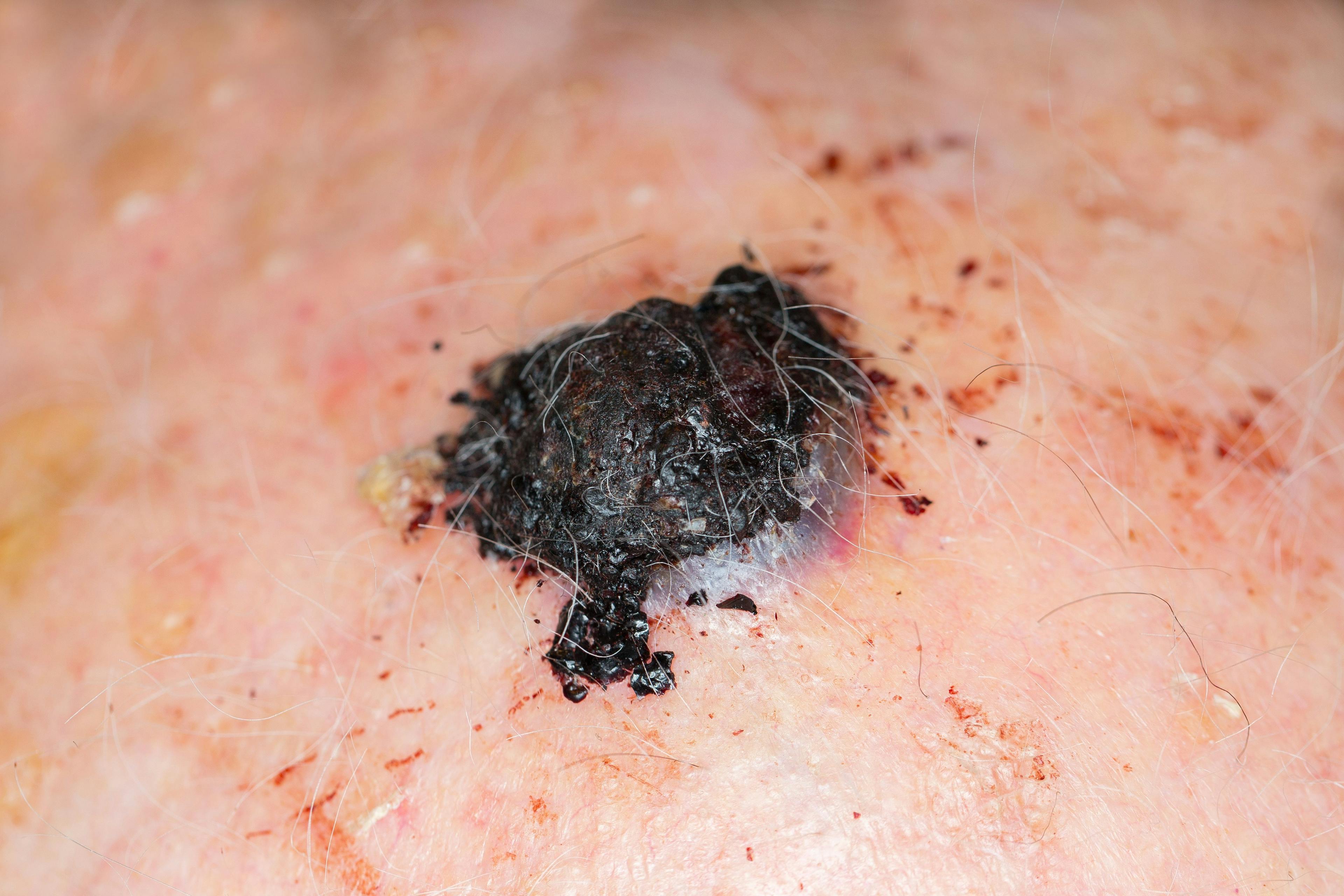
I have experienced the angst generated by countless benign nevomelanoctic nevi (Spitz, congenital, even unwanted IDN on the shoulders/chest), as well as the disproportionate investment of time and resources, the unfortunate post-operative complications, physical scars and long-term anxiety sustained by children with low-risk lesions and their families. Other benign birthmarks such as nevus sebaceous, epidermal nevus and prominent nevus simplex carry the same management challenges.
My experience as the mother of a child with a facial capillary malformation added heartfelt empathy and long-term follow-up to my perspective.2 I have also gained enough experience to rely less on the results of invasive tests than my clinical impression. I no longer biopsy typical granuloma annulare, mastocytosis, juvenile xanthogranuloma or pilomatrixoma, and I much less frequently order labs for patients on isotretinoin and methotrexate.
Hemangioma of infancy is an interesting example of the value of an evidence-based, first-line treatment for a generally benign, self-limited condition. An estimated 10% of infants develop at least one of these lesions within the first three months of life, and a significant proportion seek medical evaluation. Prior to the 2008 serendipitous discovery of propranolol, a variety of often costly higher-risk, lower-efficacy treatments were used, including radiation, surgical excision, systemic corticosteroids, vincristine and laser. Clinicians also resorted to using myriad wound-healing techniques - including becaplermin gel, at well over $1,000 for a 15 gm tube - hospitalization and narcotics to manage associated ulceration.
In the pre-propranolol era, controversy reigned about the relative risks and benefits of surgical vs medical vs no intervention. Mocking the phrase “benign neglect” helped promote a surgical approach, because “there is nothing benign about neglect.” This was countered by the concept “active non-intervention,” which was used to highlight the importance of close monitoring with intervention as warranted and based on case-by-case evaluation.
During those decades, many patient visits required high-level, time-consuming, largely non-evidence-based and exhausting shared decision-making. Pharmaceutical investment in a prospective, placebo-controlled, multicenter international pivotal clinical trial culminating in the 2014 FDA-approval of Hemangeol established a standardized, relatively simple therapeutic recommendation, and prevented significant pain, scarring and disfigurement for many thousands of children.
For non-life-threatening conditions like this, industry-funded trials are often required to quantify patient quality-of-life (QOL) benefits for the investigational treatment. I have also increasingly enjoyed the underappreciated, but very significant improvement in physician QOL that comes with a readily-available, single best treatment.
The therapeutic pipeline has not been as successful for warts and molluscum, possibly the most common of the benign, self-limited childhood skin diseases seen by dermatologists. Cry otherapy may be the most popular treatment, but one round has a 50% success rate, likely no higher than placebo.
For most children, that degree of efficacy does not offset the view, “There is no way to take the ‘cry’ out of cryotherapy.” A long list of other treatments have similar efficacy. As I often tell patients who ask for the best: If there was a single best treatment, there would not be so many choices.
I have seen many physical and emotional scars from patients treated with repeated cryotherapy, radiation and combination cantharidin (including the dreaded ring warts). The most memorable was a 4-year-old who received three rounds of bleomycin injected without anesthesia into her nares rim. She screamed from the moment I entered the room until I left, despite my promise that I would not hurt her. I especially avoid treating anogenital condylomata in children, but do screen for evidence of non-innocent transmission and evaluate for coexisting infections such as chlamydia in symptomatic children.3
I also recommend the HPV vaccine for children with widespread warts, or those persisting longer than the average two-year duration, because it suggests immunologic susceptibility to chronic or oncogenic infection. Based on the available data, the societal financial burden of these infections and their questionably effective treatments is difficult to estimate, but must be staggering.4 Fortunately, this is an incentive to develop new treatments for these unquestionably unmet medical needs.
There are currently 16 clinical therapeutic trials recruiting patients with warts5 and the same number active or completed for patients with
molluscum.6
The July of Dermatology Times features an update on these conditions, including new treatment options that hold promise for improving QOL for both patients and prescribing physicians. Â
References:
1. https://www.thelancet.com/action/showPdf?pii=S0140-6736%2808%2960379-7
2. Siefgried, E. Mark of distinction. Dermatology Times. 2012;33(4):4-6.
3. Siegfried E, Rasnick-conley J, Cook S, Leonardi C, Monteleone J. Human papillomavirus screening in pediatric victims of sexual abuse. Pediatrics. 1998;101(1Pt 1):43-7.
4. Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol.2014;134(6):1527-1534.
5. ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 2019 June 10. Available from: https://www.clinicaltrials.gov/ct2/results?cond=Warts&term=&cntry=&state=&city=&dist=&recrs=a
6. ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine
(US). 2019 June 10. Available from: https://www.clinicaltrials.gov/ct2/
results?cond=molluscum&term=&cntry=&state=&city=&dist=
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.