- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Dermatological Dilemma: Unmasking the Benzene Menace in Our Products
Author(s):
In our March publication, Winter Editor in Chief Christopher Bunick, MD, PhD, delved into the growing concern of benzene in personal care products. This commentary becomes all the more important in light of the recent findings of high levels of benzene in acne products.
There has been a surge of revelations concerning the presence of benzene, a highly toxic and carcinogenic substance, in various dermatological products commonly used by the public over the past 3 years. I underscore the gravity of this situation and urge each of you to join forces in addressing this critical issue that affects the health and safety of our patients.
Christopher Bunick, MD, PhD

I disclose that I have no financial affiliations with any entities related to this matter. My only motivation is to share crucial information and stimulate a proactive response within our dermatological community.
Benzene has long been utilized in various industries as a solvent and chemical precursor due to its catalytic properties and liquid state at room temperature. Unfortunately, it has been found to be a pervasive contaminant, with a history of hematotoxicity dating back to 1897. Studies have linked benzene exposure to significant health risks, including cancer, affecting both humans and marine life at astonishingly low concentrations in parts per billion (ppb).1
Prior studies of benzene have said “any concentration of benzene greater than 0 is not safe,”2 and that “exposure intensity in the highest exposed job was strongly related to leukemia risk with the increase starting at around 0.8 to 1.6 parts per million (ppm).”3 The CDC and World Health Organization have classified benzene as a group 1 carcinogen, placing it in the same category as asbestos, lead, and formaldehyde. I don’t think anyone in dermatology will argue about the first 2 being harmful; I remember as a kid when my elementary school closed down for a week for removal of asbestos. Placing benzene in its proper context next to asbestos and lead demonstrates why benzene must be eliminated from personal care products. As for formaldehyde, the United States Food and Drug Administration (FDA) has its proposed ban on formaldehyde and formaldehyde-releasing chemicals set for April 2024.
The alarming truth is that benzene has infiltrated numerous dermatological products, such as sunscreens, after-sun products, moisturizers, skin treatments, and other aesthetic-based formulations. For perspective, benzene concentrations in these products can range from 5000 to 60,000-fold higher than ambient air benzene exposure (~0.0003 ppm as reported by the EPA in 2010).
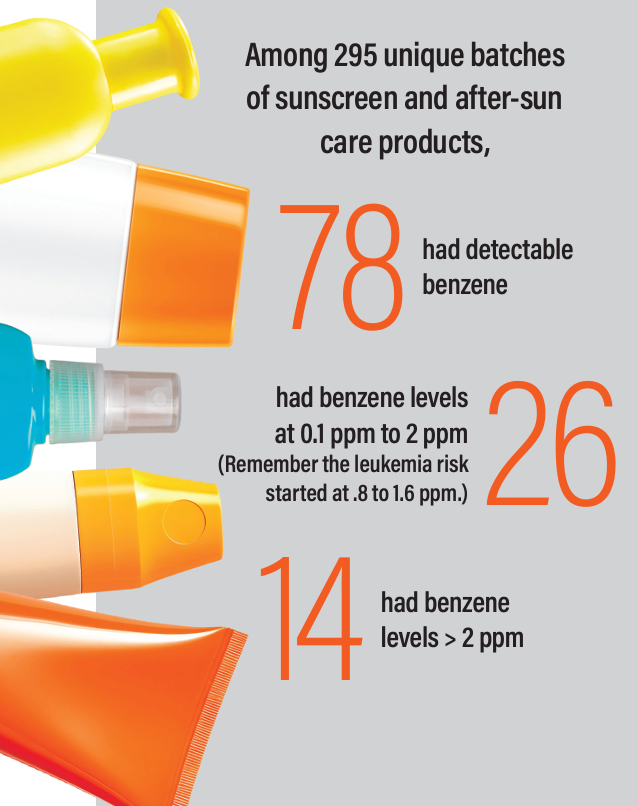
The catalyst for heightened awareness came in May 2021, when Valisure, a quality control company based out of New Haven, CT, exposed the presence of benzene in 69 different brands of sunscreen and after-sun care products.4
This revelation led to massive product recalls, including popular brands like Neutrogena and Johnson & Johnson, among others. Shockingly, internal studies conducted by these companies revealed benzene levels were significantly higher for some products (11.2 to 23.6 ppm) than what Valisure reported. It took Freedom of Information Act requests to acquire this information, emphasizing a need for greater transparency by the companies performing internal benzene analysis. Transparency is needed for the good of public health.
The complexity of the manufacturing process and supply chain is a root cause of this crisis. Dermatological products, ranging from over the counter cosmetics to advanced therapies, involve intricate manufacturing processes. However, the quality control measures implemented by manufacturers have proven inadequate, allowing benzene contamination to persist.
A timeline of recalls that started in March 2021 illustrates the extent of the problem, with hand sanitizers, sunscreens, antifungal and anti-perspirant body sprays, and even personal care items like dry aerosolized shampoos being affected. Recent research from Valisure exposed the vast variability and inconsistency in product composition of dry shampoos, highlighting the urgent need for enhanced quality control.
A citizen petition to the FDA on benzene in dry shampoos was filed in October 2022 after 148 batches of dry shampoo across 34 unique brands were sprayed in the air of a 550 cubic foot room to show short term benzene levels in the air reached 1600 ppb, and long term levels reached 36 ppb, which is 90 times higher than the EPA threshold for increased cancer risk. The EPA states a lifetime exposure of 0.4 ppb benzene in the air will likely lead to 1 additional cancer case in 100,000 exposed people.
The most important update I can provide to dermatologists is that the FDA has taken notice, under pressure from the US Congress, and the FDA acknowledges there is a benzene problem and is making major moves to correct it. This is a significant validation and victory for public safety. All dermatologists should champion truly safe products for our patients.
The FDA, recognizing the severity of the benzene issue, has taken initial steps to address benzene contamination by doing the following: (1) They have initiated recalls, (2) they have proposed benzene exposure limits, and (3) they have mandated reformulation of products containing benzene from the manufacturing process. This last point is the most significant, occurring in late December 2023. The FDA is banning certain “carbomers”—chemical polymers used in the cosmetic industry (eg, a thickening agent in topicals)—because they found some common carbomers routinely used in manufacturing had benzene levels near 5000 ppm!5 In December 2023, the FDA also released guidance for industry on how to reformulate drug products that contain carbomers manufactured with benzene. Yes, some companies will be forced by the FDA to re-formulate products in this move to eliminate benzene exposure. This signifies progress, but more substantial actions are required to ensure the safety of our patients.
A major policy change is ahead as the FDA cracks down on benzene, formaldehyde, and formaldehyde-releasing chemicals. For instance, the FDA has proposed a ban on hair-straightening products containing formaldehyde beginning in April 2024, because they have been associated with increased risks of cancer, particularly uterine cancer, and disproportionately affect Black women.6
A research study from the United Kingdom, published in December 2023, paints a real-world picture of long-term exposure to low level ambient benzene and its link to mortality. Researchers observed prospectively 393,042 UK residents with no prior stroke, myocardial infarction, or cancer history at baseline.7 They found long-term low level benzene exposure increased the risk of all-cause mortality, as well as cause-specific mortality for cardiovascular disease, cancer (leukemia, multiple myeloma, Non-Hodgkin’s lymphoma, lung cancer), and respiratory disease. Concerningly, the exposure-response curves did not show signs of a threshold or plateau over the benzene range examined, which was 0.1 to 1.0 mg/m3 (1 ppm benzene = 3.19 mg/m3, for comparison). These findings negate 2 critiques about benzene: first, companies often release statements saying, “there are no immediate health effects from benzene exposure in our products.” This study reinforces that serious adverse health effects emerge as result of long-term exposure. If there is any specialty that can understand the concept of delayed health consequences, it is dermatology, in which we regularly diagnose and treat skin cancer caused by sun exposure, often with exposure occurring decades earlier. Second, cumulative low-level benzene exposure does matter, and mortality increases measured in this study were at levels below 1 ppm average annual exposure.
I implore each of us to consider the potential impact on our patients and our profession. The long-term exposure to even low levels of benzene has been linked to increased mortality, cardiovascular diseases, and various cancers. The recent proposal by the FDA to ban benzene-containing carbomers and formaldehyde further emphasizes their commitment to eradicating harmful substances in dermatological products. Furthermore, the FDA’s actions validate the concerns over the safety of personal care products and make it impossible to sweep this problem under the rug going forward.
In conclusion, the time for collective action is now. We must stay informed, engage in discussions within our community, and advocate for stringent quality control measures. Our patients entrust us with their well-being, and it is our responsibility to ensure that the products we use and recommend in our practices meet the highest standards of safety and quality.
Let us stand united in safeguarding the health of our patients and upholding the integrity of dermatology as a field committed to the highest standards of care.
References
- NCI thesaurus: Benzene. National Institutes of Health. Accessed February 21, 2024. https://ncit.nci.nih.gov/ncitbrowser/ConceptReport.jsp?dictionary=NCI_Thesaurus&ns=NCI_Thesaurus&code=C302.
- Smith MT. Advances in understanding benzene health effects and susceptibility. Annu Rev Public Health. 2010;31:133-following148. doi:10.1146/annurev.publhealth.012809.103646
- Glass DC, Gray CN, Jolley DJ, Gibbons C, Sim MR, Fritschi L, Adams GG, Bisby JA, Manuell R. Leukemia risk associated with low-level benzene exposure. Epidemiology. 2003 Sep;14(5):569-77. doi: 10.1097/01.ede.0000082001.05563.e0. PMID: 14501272.
- Petronelli M. Valisure highlights controversy of benzene contamination in sunscreen products. Dermatology Times. May 26, 2021. Accessed February 27, 2024. https://www.dermatologytimes.com/view/valisure-highlights-controversy-of-carcinogens-in-sunscreen
- Bader K. FDA provides new industry recommendations for reformulation of drug products containing carbomers manufactured with benzene. Dermatology Times. January 11, 2024. Accessed February 27, 2024. https://www.dermatologytimes.com/view/fda-provides-new-industry-recommendations-for-the-reformulation-of-drug-products-containing-carbomers-manufactured-with-benzene
- Bader K. Proposed FDA ban of formaldehyde in hair relaxers: what comes next?. Dermatology Times. November 6, 2023. Accessed February 27, 2024. https://www.dermatologytimes.com/view/proposed-fda-ban-of-formaldehyde-in-hair-relaxers-what-comes-next-
- Villeneuve PJ. Long Term Exposure to Ambient Benzene and Mortality. Am J Respir Crit Care Med. 2024 Feb 1. doi: 10.1164/rccm.202401-0005ED. Epub ahead of print. PMID: 38301235.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.