- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Dermoscopy Falls Short in Diagnosing Demodex
Author(s):
Dermoscopy cannot diagnose D folliculorum proliferation but can reveal specific findings in patients with papulopustular rosacea.
Dermoscopy, by itself, is not a strong enough tool for diagnosing Demodex folliculorum mite proliferation in papulopustular rosacea, according to the results of a study recently published in Clinical and Experimental Dermatology.1
Rosacea is estimated to affect more than 16 million Americans, according to the National Rosacea Society.2 And mask wearing during the COVID-19 pandemic appears to have worsened rosacea in untreated patients, according to findings from a study published in Dermatologic Therapy.3
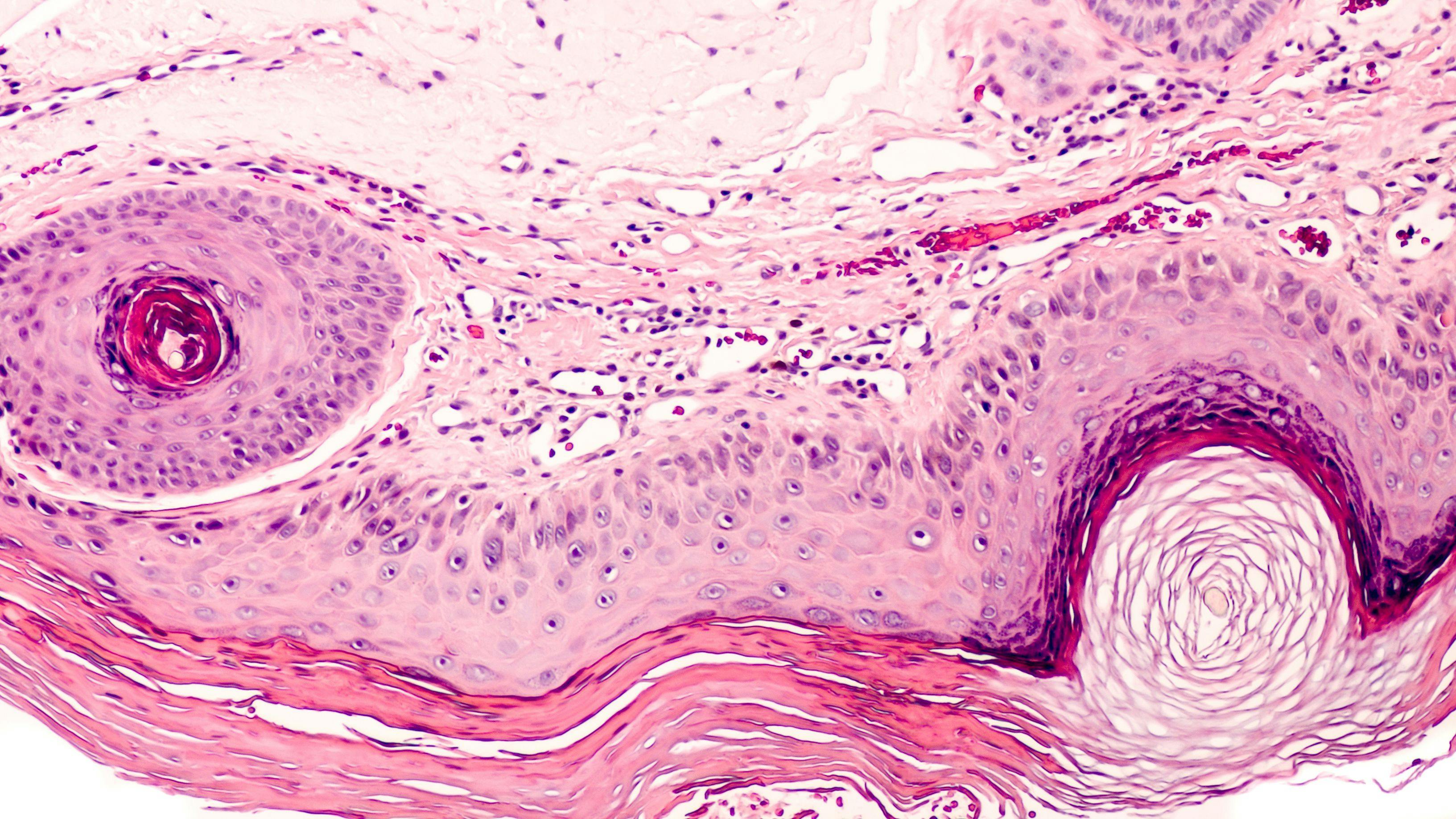
“Although the diagnosis of rosacea is mainly clinical, dermoscopy may contribute to the diagnostic process,” study author Ilaria Trave, MD, a dermatologist at the University of Genoa, Ospedale Policlinico San Martino in Italy, told Dermatology Times®. “Moreover, dermoscopic indicators of Demodex mite proliferation, such as Demodex tails—gelatinous, whitish creamy threads, 1 to 3 mm in length—and Demodex follicular openings—dilated follicular openings containing round, amorphic, greyish light-brown plugs surrounded by an erythematous halo—are usually evaluated in primary demodicosis, such as pityriasis folliculorum, and are less studied in papulopustular rosacea.”
Trave and colleagues prospectively studied dermoscopy images and skin surface biopsies in 60 Caucasian male and female patients with papulopustular rosacea with almost clear, mild and moderate disease.
The images and biopsies revealed that dermoscopy is a valid tool for identifying papulopustular rosacea in an early stage, with the most frequent dermoscopic features being yellow dots, vascular polygons, and follicular scales.
“We found specific dermoscopic findings of mild papulopustular rosacea, such as tiny papules and pustules that are not recognized by the naked eye; polygonal vessels, or vascular polygons; yellow dots, or dilated follicular infundibula filled with keratotic material and/or sebum; and follicular scales, which are dry and pale scales,” Trave wrote.
The investigators report that D folliculorum mites were found in 20 of the 60 patients with standardized skin surface biopsy. But patients with the mites were no more likely to have more Demodex tails or follicular openings than patients without the mites.
Compared with standardized skin surface biopsy, dermoscopy showed 50% sensitivity and 77.5% specificity for D folliculorum mite infestation diagnoses.
“This study shows that papulopustular rosacea presents specific dermoscopic findings and that some of them, such as Demodex follicular openings, follicular scales, follicular pustules, and honeycomb pigment pattern, are more frequent in moderate than almost-clear rosacea,” Trave noted. “Regarding demodicosis in papulopustular rosacea, we show that dermoscopy alone is not a strong enough method for diagnosis, and that it needs to be confirmed by means of a standardized skin surface biopsy or reflectance confocal microscopy.”
Standardized skin surface biopsy is a sampling method in which 1 cm2 of the superficial layer of the stratum corneum and its follicular content is obtained for analysis. These samples were examined with an optical microscope (x 10 and x 40 magnifications). Samples with x 5 Demodex/cm2 or more are considered Demodex positive, according to Trave.
“Dermoscopy might be a valuable tool for dermatologists in case of doubtful diagnoses of facial dermatitis,” the authors wrote.
The absence of a control group and exclusion of severe papulopustular rosacea cases are potential study limitations.
Disclosure:
Trave reports no conflicts of interest.
References:
1. Trave I, Micalizzi C, Gasparini G, Cozzani E, Parodi A. Dermoscopy of papulopustular rosacea and comparison of dermoscopic features in patients with or without concomitant Demodex folliculorum. Clin Exp Dermatol. Published online May 13, 2021. doi:10.1111/ced.14731
2. Rosacea Awareness Month highlights new treatment options for life-disruptive disorder affecting 16 million Americans. Press release. National Rosacea Society. April 1, 2020. Accessed June 7, 2021. https://www.rosacea.org/press/2020/april/rosacea-awareness-month-highlights-new-treatment-options
3. Damiani G, Gironi LC, Grada A, et al. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): multi-center, real-life, telemedical, and observational prospective study. Dermatol Ther. 2021;34(2):e14848. doi:10.1111/dth.14848

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.