- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
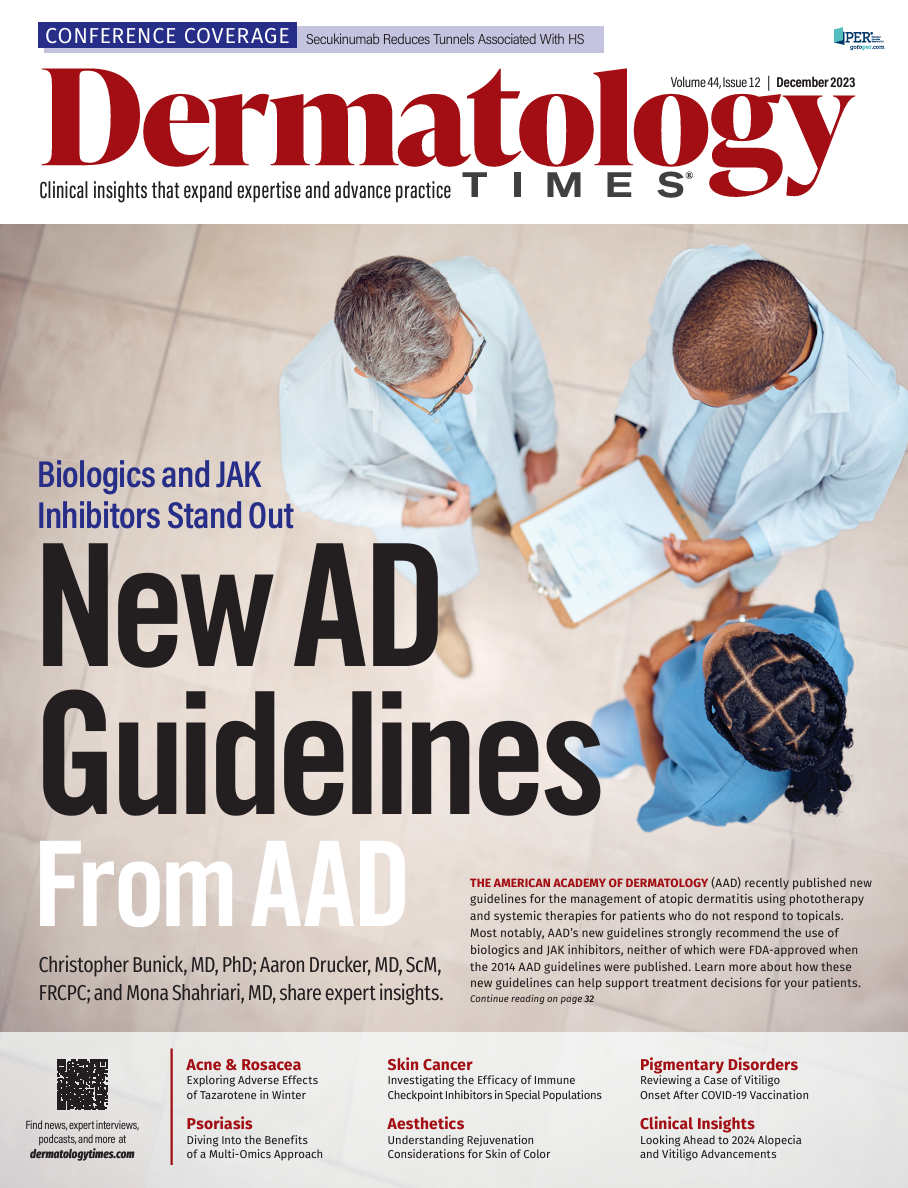
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Emergence of Antifungal-Resistant Dermatophyte Infections
Author(s):
Cognizance and certain clues may help dermatologists in recognizing antifungal-resistant dermatophyte infections.
cunaplus/Adobe Stock

Dermatophyte infections, involving the skin, hair, and nails, affect approximately 20% to 25% of the global population. They may cause pain, pruritus, dyspigmentation, hair loss, and secondary bacterial infections, as well as affect psychosocial interactions and quality of life. Topical antifungals may be sufficient for treating dermatophyte skin infections and mild onychomycosis cases. However, oral antifungal therapy is necessary for treating tinea capitis, moderate to severe onychomycosis cases, treatment failures, and extensive dermatophyte skin infections. Recently, antifungal-resistant dermatophyte infections, which are resistant to topical antifungals and oral terbinafine, have emerged as a serious threat in the United States.
In 2023, multiple dermatophyte cases due to Trichophyton indotineae were reported in the United States.1 T indotineae is a new dermatophyte strain that is often resistant to oral terbinafine and causes extensive tinea corporis, cruris, or faciei cases. Also this year, there have been reports of onychomycosis cases due to Trichophyton rubrum2 resistant to oral terbinafine and oral itraconazole.3
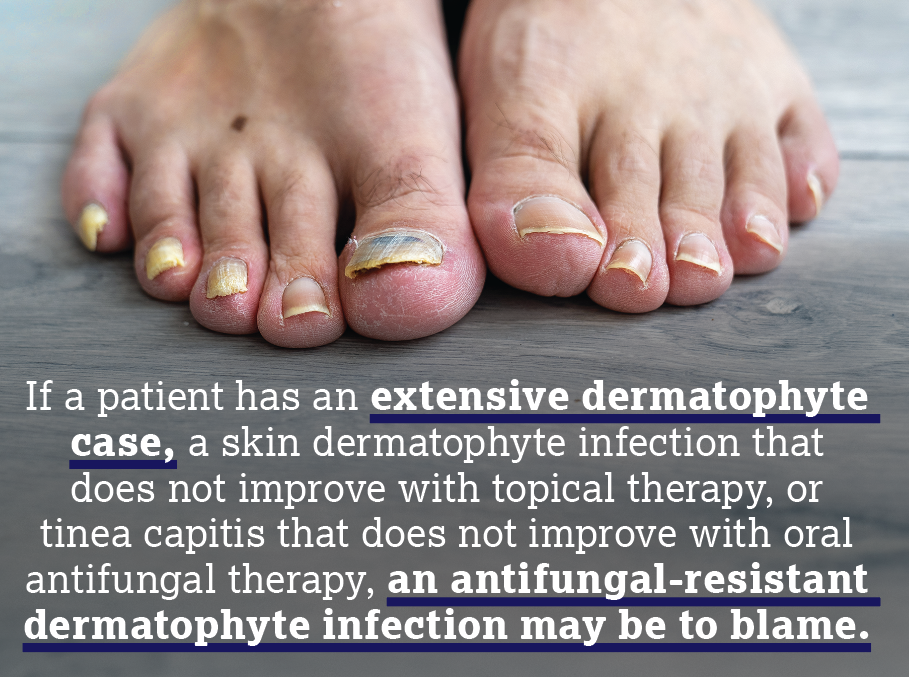
Cognizance and certain clues may help dermatologists in recognizing antifungal-resistant dermatophyte infections. If a patient has an extensive dermatophyte case, a skin dermatophyte infection that does not improve with topical therapy, or tinea capitis that does not improve with oral antifungal therapy, an antifungal-resistant dermatophyte infection may be to blame. Risk factors for T indotineae include immunocompromised state; recent travel to the Middle East or South Asia, where this strain is prevalent; and contact with someone infected with T indotineae. However, immunocompetent people, patients without recent travel to endemic areas, and patients without contacts may be affected. Thus far, there are no clinical features that distinguish terbinafine-resistant T rubrum onychomycosis from terbinafine-sensitive ones, but patients with terbinafine-resistant T rubrum onychomycosis will not improve after the FDA-approved terbinafine course (3 months).
Unfortunately, most local, commercial, and academic laboratories usually do not have the tools to diagnose these antifungal-resistant dermatophyte infections. These infections require specialized testing. For example, confirmation of T indotineae requires genetic sequencing. Using a culture alone will usually report T indotineae as Trichophytonmentagrophytes or Trichophyton interdigitale, causing misdiagnosis and negatively influencing treatment decisions. Polymerase chain reaction (PCR) testing is often required to diagnosis terbinafine-resistant T rubrum onychomycosis cases.3 If an antifungal-resistant dermatophyte infection is suspected, dermatologists are recommended to contact local and health departments for assistance or the CDC at FungalOutbreaks@cdc.gov.
Since these antifungal-resistant dermatophyte infections have newly been recognized in the United States, they are first being characterized and there are no written guidelines or consensus papers. Available evidence for cases reported globally, as well as for the few cases reported in the United States, suggests that long treatment courses with oral itraconazole, typically for longer than 3 months, may be needed. Itraconazole has a more extensive adverse effect profile compared with terbinafine, and many more drug-drug interactions, which may be a challenge, particularly in older adults who often have comorbidities and are taking concomitant medications. Monitoring itraconazole serum levels may help mitigate against adverse events and ensure that drug levels are not too high or low.
Choice of medication may be even more complicated. There are reports of itraconazole-resistant dermatophyte infections. For these infections, particularly for organisms also resistant to terbinafine, voriconazole and posaconazole are other options. As these medications are rarely utilized by dermatologists, infectious disease specialists may be consultants for management.
Clearly, emergence of antifungal-resistant dermatophyte infections is a major problem, given that we have so few alternative drugs and given that new drug approvals may take many years. Therefore, we as a dermatology community must do everything we can to prevent antifungal resistance. Empiric treatment of dermatologic conditions is thought to promote resistance. Mycological testing is easy to do, and there are a number of available options. Potassium hydroxide staining with microscopy on scrapings is the fastest and most cost-effective diagnostic option. The disadvantages are that this technique cannot identify the causative organism, the laboratory must be Clinical Laboratory Improvement Amendments certified, and it is expertise dependent. A nail clipping with histopathology with periodic acid-Schiff or Gomori methenamine-silver staining is easy to do and has high sensitivity, but the fungal strain cannot be identified. Fungal culture is the only technique that identifies viability of the pathogen. It may also identify the causative organism, but it often takes several weeks for results, and there is a high false negative rate. DNA-based techniques such as PCR are also available for mycologic confirmation. The technique has very high sensitivity and can identify the causative organism, but it may also identify contaminants and has high cost.
Another way to help prevent antifungal resistance is to educate patients and nondermatologists on the dangers of prescribing antifungal-corticosteroid combination topicals for fungal infections.4 Corticosteroid creams may initially improve the clinical appearance of a dermatophyte infection and reduce itch, but they may also mask the correct diagnosis, impact local immune regulation, and worsen dermatophyte infections. Efforts to educate nondermatologists and patients against empiric treatment and self-diagnosis, respectively, may improve patient outcomes and halt the spread of antifungal-resistant dermatophyte infections.
Antifungal-resistant dermatophyte infections are real and something we need to worry about. Dermatologists can take additional steps to prevent further resistance and prevent spread. Empiric treatment and inappropriate use of antifungals can select for antifungal resistance, making antifungal stewardship increasingly important.
Shari R. Lipner, MD, PhD, is an associate professor of clinical dermatology, associate attending physician, and director of the Nail Center at the New York-Presbyterian Hospital/Weill Cornell Medical Center in New York, New York. She is a member of the American Academy of Dermatology, Women’s Dermatologic Society, Council for Nail Disorders, and American Dermatological Association, and is chair of multiple committees. She is the former president of the Dermatologic Society of Greater New York and is the president of the New York State Society of Dermatology and Dermatologic Surgery. She is an internationally recognized nail expert who lectures nationally and internationally, and has authored more than 15 book chapters and over 370 peer-reviewed publications.
Financial disclosures: Lipner has served as a consultant for Ortho-Dermatologics, BelleTorus Corporation, Eli Lilly and Company, and Moberg Pharma.
Lipner has no conflicts of interest relevant to the content of the submission.
References
- Caplan AS, Chaturvedi S, Zhu Y, et al. Notes from the field: first reported U.S. cases of tinea caused by Trichophyton indotineae - New York City, December 2021-March 2023. MMWR Morb Mortal Wkly Rep. 2023;72(19):536-537. doi:10.15585/mmwr.mm7219a4
- Hwang JK, Bakotic WL, Gold JAW, Magro CM, Lipner SR. Isolation of terbinafine-resistant Trichophyton rubrum from onychomycosis patients who failed treatment at an academic center in New York, United States. J Fungi (Basel). 2023;9(7):710. doi:10.3390/jof9070710
- Elewski B. A call for antifungal stewardship. Br J Dermatol. 2020;183(5):798-799. doi:10.1111/bjd.19387
- Benedict K, Gold JAW, Wu K, Lipner SR. High frequency of self-diagnosis and self-treatment in a nationally representative survey about superficial fungal infections in adults—United States, 2022. J Fungi (Basel). 2023;9(1):19. doi:10.3390/jof9010019
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.