
- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Helping Patients Navigate New Environments to Manage Atopic Dermatitis
Author(s):
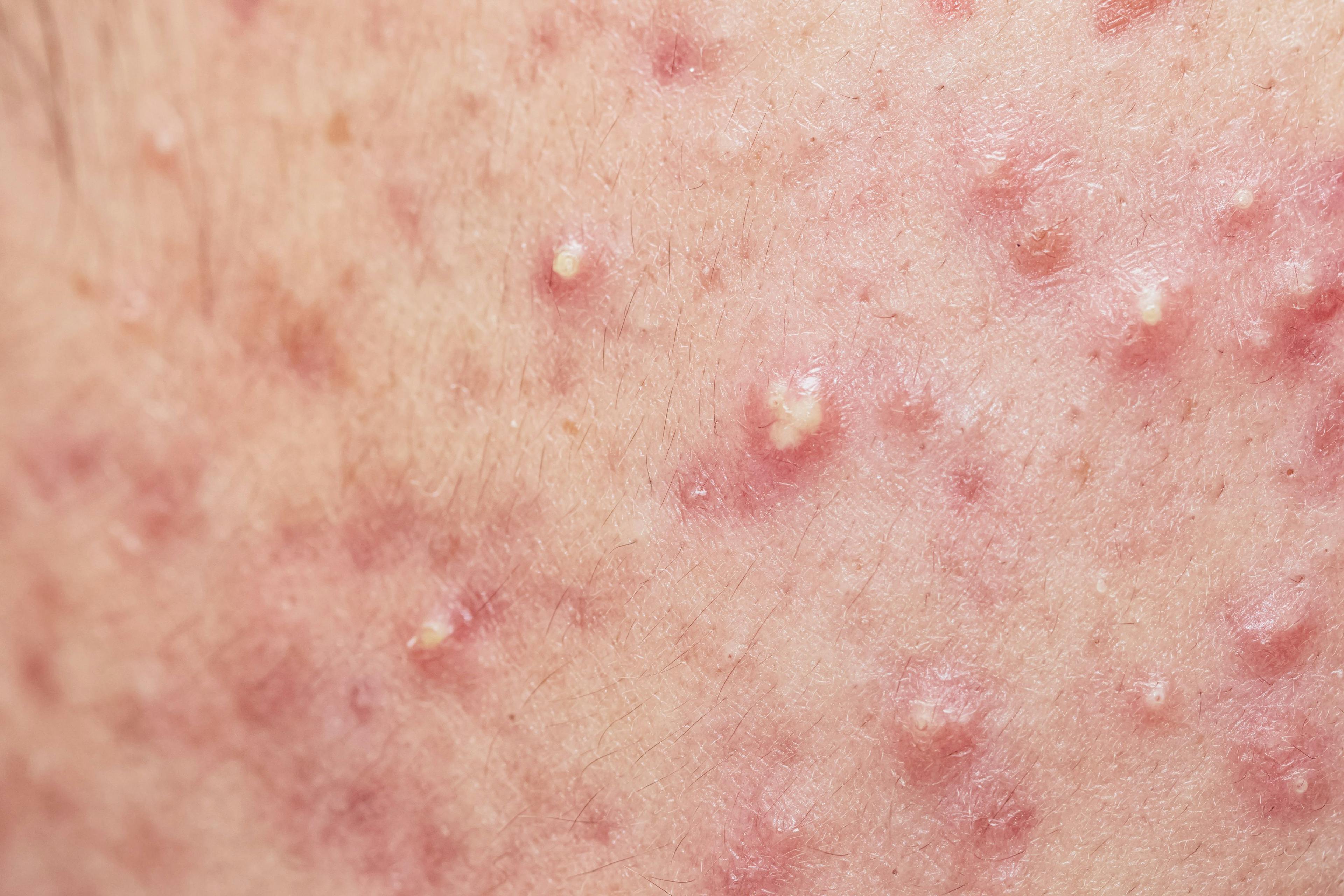
Roundtable participants shared 10 different considerations to make for a patient, like this 23-year old woman, with a new environment and lifestyle.
Evaluating patients’ individual needs is key to atopic dermatitis (AD) treatment—a common theme discussed during a recent series of Dermatology Times Case-Based Roundtable meetings for clinicians across the US to discuss practical treatment solutions tailored to challenging patient cases presented.
TJ Chao, MPAS, PA-C, practices at Atlanta North Dermatology in Woodstock, Georgia. He moderated a discussion including the case of a 23-year-old Caucasian woman with a history of moderate AD for more than 20 years on her arms, legs, face, and neck. Now, patches present as erythematous, eczematous, scaling patches only on her face and neck. There is some lichenification and hyperpigmentation on the face and neck.
Case Background
The patient utilized topical steroids for almost 18 years, but the condition was not consistently stable with a body surface area (BSA) of 12% and Investigator Global Assessment (IGA) score of 3. When she was 19 years old, she started dupilumab (Dupixent) and did well for a few years with a sustained level of complete clearance. However, over the last year, flare-ups started, and she was prescribed topical steroids. Topical steroids slowed down flares for 2 weeks before they were exacerbated again. The patient was prescribed fluticasone propionate 0.05% cream twice a day for 2 weeks and pimecrolimus 1% cream twice a day, and facial patches have not resolved. Due to occasional flares, the patient commenced ruxolitinib twice daily on the face and neck. She is currently in a master’s program at a major university in Georgia and lives in student housing, which concerns the patient because of dust mites, dusty air conditioners, and dry air potentially exacerbating her condition.
Follow-Up Appointments
The patient was followed up with 2 months after starting ruxolitinib (Opzelura) cream alongside dupilumab. In follow up, she stated that her AD noticeably cleared after a few weeks and has been clear for 1 month. She states that she continued the ruxolitinib cream twice daily to the face and neck for added assurance.
At her next visit 3 months later, the patient was still clear on dupilumab use with BSA = 0% and IGA = 0.
She is still using ruxolitinib for occasional flaring on the face and neck, but only used it twice daily for a few days whenever flares developed on her face, neck, arms and legs.
Considerations for Clinicians
Roundtable participants shared 10 different considerations to make for a patient, like this 23-year old woman, with a new environment and lifestyle.
1. Evaluate the Patient’s Routines
The patient believes dust mites and her mattress might be causing the rashes. Consider addressing this concern and exploring potential environmental triggers. Ask the patient about skin care routines and any prescriptions or over-the-counter products that may have irritants in them.
2. Review Medication History
The patient has been on dupilumab for several years, but flares occurred suddenly. Since the patient flared after years of being clear on dupilumab, consider the possibility of contact dermatitis. Patch testing and exploring exposure to irritants like essential oils, incense, or other environmental factors could be triggers.
3. Utilize the Power of POEM
Roundtable participants commended the Patient-Oriented Eczema Measure (POEM) questionnaire for patients to better articulate their improvement or challenges. POEM asks 7 questions including how many days in the last week skin has been itchy, how many nights of sleep were disturbed, and how many days flares have bled. The calculated score out of 28 points indicates whether the patient with atopic dermatitis is clear or almost clear, mild, moderate, severe, or very severe.
4. Switch Medications
Some dermatology clinicians in the roundtable mentioned the option of switching from dupilumab to tralokinumab (Adbry) or JAK inhibitors like upadacitinib (Rinvoq). It was noted that some patients have shown improvement with these changes.
5. Explore Ruxolitinib
Ruxolitinib was suggested for use in conjunction with dupilumab. The roundtable of clinicians discussed strategies to obtain ruxolitinib, including navigating insurance barriers and utilizing patient assistance programs.
6. Educate on Topical Treatments
Discuss the use of ruxolitinib as a topical treatment, emphasizing its efficacy in managing redness and itching. Clarify any warnings or concerns associated with the medication.
7. Communicate Clearly With Patients
Effectively communicate with the patient about treatment options, addressing their concerns, and ensuring they understand the rationale behind the prescribed regimen. Each AD patient has different lifestyles, concerns, and adherence capabilities.
8. Long-Term Monitoring
Plan for regular follow-up appointments to assess the patient’s progress, adjust treatment as needed, and ensure ongoing support for managing atopic dermatitis. If the patient is temporarily living away from home or is in a busy chapter, like this 23-year-old grad student, consider telehealth options for patient convenience.
9. Consider Alternatives
In cases where ruxolitinib may be challenging to obtain, explore alternative topical treatments like tapinarof (Vtama) or roflumilast (Zoryve), considering cost-effectiveness and patient response.
10. Ensure Patient Satisfaction
Regularly assess the patient’s satisfaction, quality of life, and perceived improvement. Adjust the treatment plan based on their feedback and overall well-being.
See other considerations for complex cases from the conversation Chao moderated.












Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.

