- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
How to Tackle Challenging Cases in Dermatology
Author(s):
Dermatologists have to face down dermatologic diseases and conditions that test their skills in diagnosis, treatment, and management. One expert shares some interesting dermatology cases that may stump even the veteran dermatologist and how to find solutions.
Dermatologists regularly see a broad range of skin diseases and conditions not all of which may have a typical text-book presentation. This can sometimes lead to confusion and diagnostic ambiguity and can often require extensive differential diagnoses as well as meticulous diagnostic workup to help elucidate the case. Matthew J. Zirwas, MD, recently presented on a number of these skill-stretching cases at Maui Derm NP + PA 2022 Summer Conference.
He is an associate professor at Ohio University Heritage College of Medicine in Athens, Ohio. Zirwas offered these examples of cases that challenge even the most experienced dermatologists and how he solved them.
The Patient with the Hands and Feet
A few years ago, Zirwas followed the clinical journey of a 66-year-old female patient who presented in his clinic with a 1-year history of a pruritic rash on the arms, hands, and chest. Biopsy revealed a spongiotic dermatitis and patch testing showed a strong allergy to budesonide, a marker for steroid allergy. The patient was subsequently switched to low allergenicity topical desoximetasone and systemic dexamethasone steroid treatment.
After an initial slight improvement of symptoms, the patient presented with a severely swollen and tender left arm. Culture revealed an MRSA infection, and negative for clot. After failing trimethoprim sulfamethoxazole, minocycline, and cephalexin treatment regimens, the patient finally responded to a 10-day course of linezolid and improved for 6 months. The patient relapsed again but this time responded to trimethoprim sulfamethoxazole and dexamethasone therapy on which she improved for another 6 months.
The clinical journey of the patient continued with a diagnosis of lung cancer which was treated with surgery without the need for chemotherapy, with the exanthem resolving about 1 year after the cancer. However, the patient soon returned and presented with the rash on the face, central chest, arms, and scalp, with another biopsy revealing dermatitis.
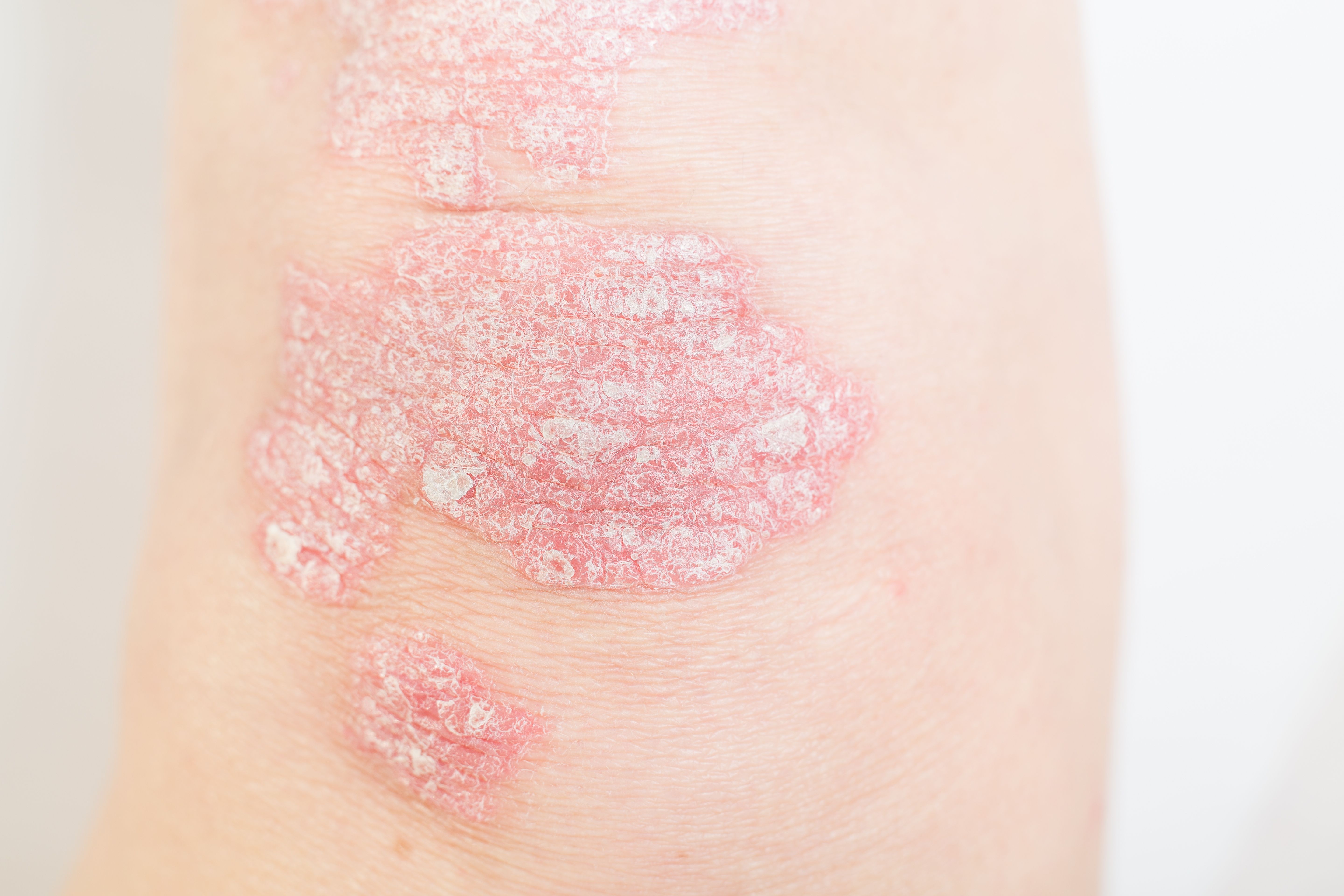
Symptoms improved with prednisone but flared again 2 months later. The patient was then diagnosed with breast cancer and was subsequently treated with surgery, radiation, and chemotherapy. The rash cleared for about 1 year after which it recurred on the neck, chest, and hands with prominent involvement of the fingernails and periungual areas causing extreme pain and itch. Unfortunately, not much improvement was achieved with systemic steroids and antibiotics, and the rash further spread to the soles of the feet with vesicle formation causing severe pain and immobility.
As the patient met the AAD criteria for atopic dermatitis, a course of dupilumab (Dupixent, Sanofi and Regeneron Pharmaceuticals) was started for a duration of 3 months after which the symptoms worsened. Dupilumab was discontinued and cyclosporine 300 mg/day started with some success. Unfortunately, due to tremors, cyclosporine was also discontinued, and the patient then received ixekizumab for presumed psoriasis, which was also discontinued due to tremor relapse.
Zirwas then started the patient on medium dose (2.25 mg/day) dexamethasone and apremilast (Otezla; Amgen). After a worsening of symptoms, apremilast was discontinued and the dexamethasone dose was increased to 4.5 mg/day. Continuing with dexamethasone, Zirwas also administered methotrexate (MTX) 10 mg/week to the patient, upon which symptoms worsened.
Oral tacrolimus 2 mg/bid was then started which proved to be moderately helpful but the tremors recurred. After discontinuing tacrolimus, the patient received upacitinib 15 mg/day and valacyclovir 500 mg/qid. Finally, the patient’s symptoms dramatically improved with upacitinib (Rinvoq; AbbVie) therapy and laboratory results have stabilized.
Zirwas believes the patient had a chronic, pruritic, spongiotic, non-contact dermatitis, sparing the groin and axilla. Although it is very difficult to know exactly what the patient really has, Zirwas said that the patient does meet the criteria for atopic dermatitis (AD).
“Approved for the classic Th2 disease atopic dermatitis, and Th1 diseases rheumatoid arthritis and psoriatic arthritis, Janus inase (JAK) inhibitors have a wide spectrum of activity and are a reasonable go-to when you have somebody you cannot get off of systemic steroids,” Zirwas said.
The Patient with the Pants
Another interesting case involved a 50-year-old patient who presented with severe dermatitis primarily affecting the backs of the legs, although it spread all over at times for approximately one year in duration. No significant improvements could be achieved with clobetasol, prednisone, dexamethasone, and deoximetasone therapy. After patch testing showed to be strongly positive for textile dyes (patient often wears dark blue or black yoga pants), the patient was appropriately instructed on avoidance and was started on cyclosporine which was appropriately tapered for relief while waiting for avoidance to become effective.
The patient improved dramatically but developed renal abscesses and sepsis, leading to the discontinuation of cyclosporine. After continuing to improve with avoidance, the patient experienced a widespread severe flare 6 months later in the summer with particular severity on the backs of the legs.
According to Zirwas, the severe flare was likely due to the patient’s profuse sweating releasing the dye from a new pair of jeans, and a secondary ID reaction. Symptoms cleared with a tapering regimen of prednisone as well as continued avoidance of dyes. Unfortunately, the patient flared and symptoms got worse throughout the summer with the backs of the legs being the most severely affected, however, systemic steroid therapy could only lead to a temporary improvement.
“The patient claims she is avoiding dyes, but I suspect she is not compliant. Nevertheless, I decide to believe her, which would mean she has atopic dermatitis and not contact dermatitis, so I initiated dupilumab which cleared her symptoms,” Zirwas said.
The patient did not have childhood dermatitis, no significant personal history of atopy, no flexural predominance, and patch testing that fit perfectly with the distribution of the dermatitis. According to Zirwas, the question remains as to whether the patient had atopic dermatitis all along or did dupilumab prove effective for contact dermatitis.
The Patient with Skin Cancer
A 72-year-old female patient presented with a history of multiple eruptive keratoacanthomas on the lower legs and a widespread rash on the body. Patch testing showed positive for formaldehyde and betaine-related lathering ingredients, which correlated well with the distribution of the dermatitis. Unfortunately, avoidance proved ineffective but according to Zirwas, the symptoms and clinical picture met the American Academy of Dermatology (AAD) criteria for AD.
“We initiated dupilumab therapy and the dermatitis cleared. The hope is that it will decrease the rate of keratoacanthomas since recent reports have shown resolution of warts and molluscum contagiosum,” Zirwas said.
Unfortunately, however, the patient continued to develop keratoacanthomas on the lower legs in the rhythm of about 1 per month, with significant dermatitis present in the area of the lesions. Dupilumab was discontinued and methotrexate (MTX) was initiated. After an initial flare of the dermatitis, the patient improved following 8 weeks of MTX treatment.
Disclosures
Zirwas is a speaker for Genentech, Novartis, Sanofi, and Regeneron Pharmaceuticals, Inc. He is a consultant for Sanofi/Regeneron Pharmaceuticals, Fitbit, L’Oréal, LEO Pharma, Pfizer Inc, Eli Lilly and Company, Arcutis Biotherapeutics, Ortho Dermatologics, Sol-Gel Technologies, Bausch Health, and EPI Health Inc. He is an investigator for Sanofi/Regeneron Pharmaceuticals, LEO Pharma, Janssen Pharmaceuticals Companies of Johnson & Johnson, Incyte, Vyne Therapeutics Inc, UCB, Pfizer Inc, Eli Lilly and Company, Asana Biosciences LLC, Avillion LLP, AbbVie, Edesa Biotech Inc, Galderma, Dermavant Sciences, Arcutis Biotherapeutics Inc, EPI Health Inc, and Concert Pharmaceuticals Inc. He is part owner of AsepticMD.
Reference
Desai S, Herbert A, Rosen T, and Zirwas M. Challenging cases. Presented at Maui Derm NP + PA 2022. Held June 23 – 25, 2022 in Colorado Springs, Colorado, and virtual.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.