- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
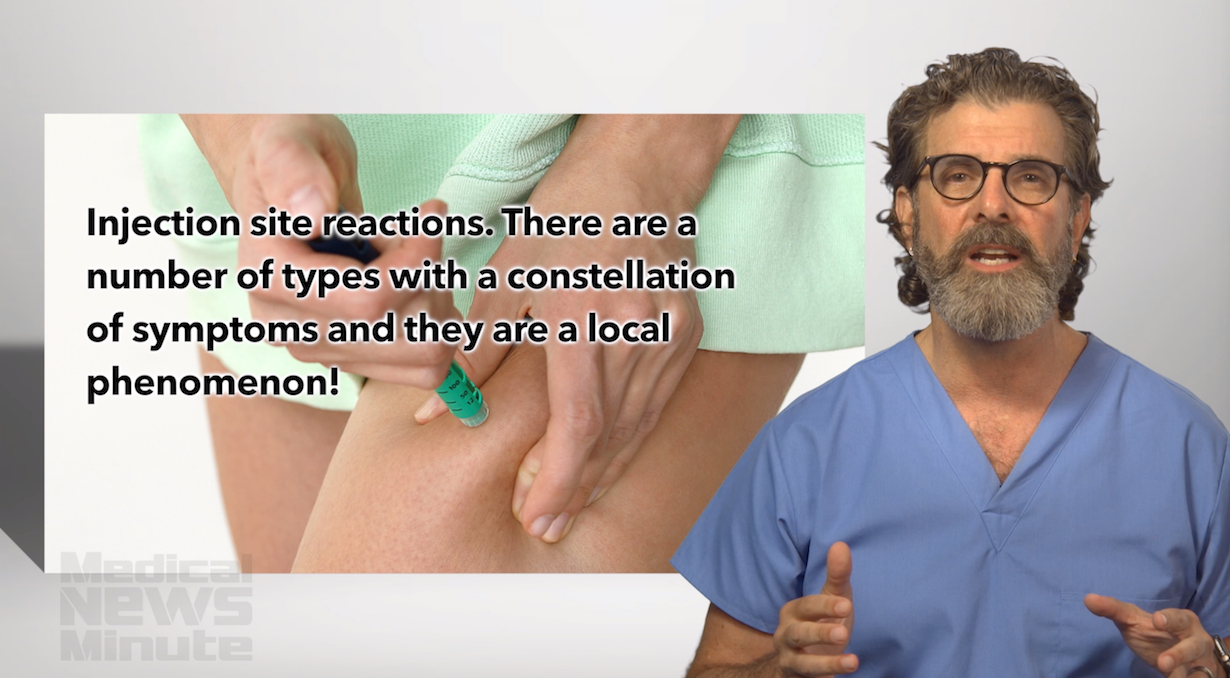
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
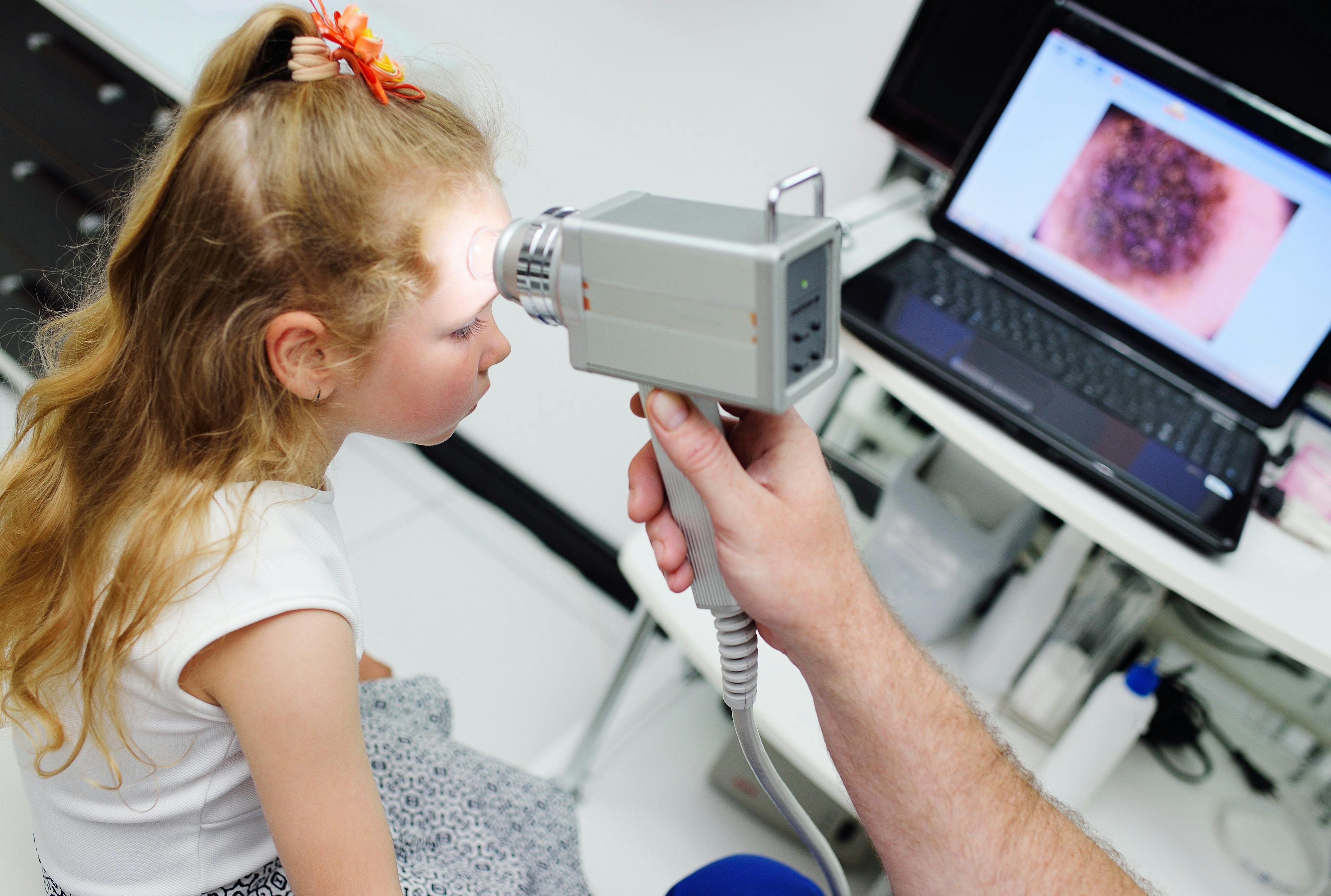
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
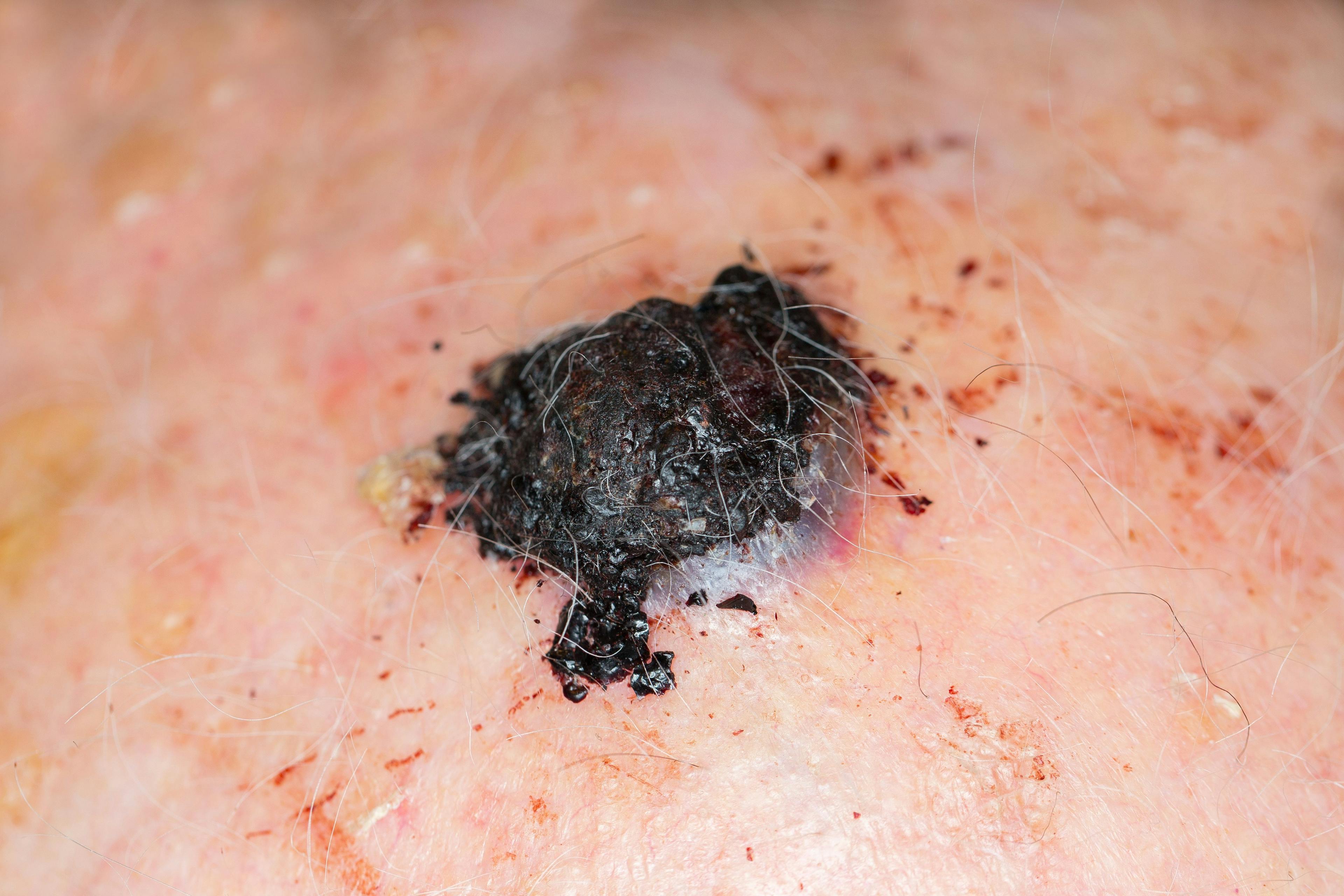
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Inflammation and aging
Author(s):
‘Inflammaging’ is real, says one expert, and can result from chronic inflammation, cell senescence and other internal processes.
Dr. Schell

While topical products and treatments can address visible signs of skin aging, antiaging regimens also must address internal processes such as chronic inflammation and cell senescence.
That’s according to Pamela J. Schell, Psy.D., MSN, ARNP, DNC, who spoke on this issue at the Fall 2018 Cosmetic Bootcamp. Dr. Schell says evidence supporting the role of chronic inflammation in human aging has grown. Researchers have even coined a term for the process - "inflammaging." Dr. Schell is director of Werschler Aesthetics in Spokane, Washington.
"Clients always ask me why I look so young for my age. Part of that is, I take care of myself from the inside out. It's not just about getting your Botox (abobotulinum toxin A, Allergan) and Retin-A (tretinoin, Ortho Dermatologics)," she says. Much of the battle, says Dr. Schell, occurs within the body. "And now we're finding out that that really is much more the case than we thought."
Antiaging dermatologic procedures provoke controlled acute inflammation. Conversely, she says, chronic inflammation is long-term, low-grade inflammation that leads to increased levels of pro-inflammatory cytokines including TNF-A, interleukin (IL)-1B and IL-6, even in the skin, which has its own immune response system. Processes affected by inflammaging range from DNA replication to cell senescence, immunosenescence and the skin-gut axis, she adds.
"Our guts do a lot for us - including making many hormones," says Dr. Schell. The microbiome, which exists mainly in the gut, is also responsible for maintaining a balance of healthy versus unhealthy bacteria - although science has not yet identified which bacteria are which, for which patients. Such determinations depend partly on genetics, she says. "We don't completely understand everything that our gut microbiome does for us. But we know its function decreases with aging, and it is affected by this chronic low-grade inflammatory process." The gut microbiome of elderly patients shows decreased diversity, she adds, with research showing lower amounts of anti-inflammatory microbiota such as Clostridium cluster XIVa, Bifidobacterium spp. and Faecalibacterium prausnitzii.1
Lifestyle Choices
Even in developing regions, says Dr. Schell, the burden of avoidable age-related illnesses has grown as people worldwide eat more processed food and exercise less. Other harmful lifestyle choices include smoking, which increases levels of several pro-inflammatory cytokines and, more importantly, reactive oxygen species. "Those are all things that we see when the immune system is stressed and trying to fight something."
Similar dynamics occur in the mouth, as diminished protection against bacterial species that occurs with age can lead to periodontal disease and chronic low-grade inflammation that spreads throughout the cardiovascular system, resulting in cardiovascular disease.
Healthy dietary choices can include the Mediterranean diet, the calorie restriction diet and the ketogenic diet, she says. "I don't know if the keto diet is going to be a flash in the pan or a long-term solution." Larger studies have suggested that a modified Mediterranean diet that includes some ketogenic elements may be better, she explains.
Dr. Schell also recommends supplementing gut microbiota with probiotics and prebiotics (food sources, such as fiber, for probiotics). Because it remains unclear which probiotic species provide maximum benefits in which patient groups, says Dr. Schell, gastroenterologists and rheumatologists often recommend rotating several strains monthly.
Stress Affects the Skin
Stress also impacts the skin through the brain-skin connection. Along with immediately perceiving external stressors such as heat, cold, pain and mechanical tension, she says, the skin is a target of stress responses. Various receptors transmit these external signals to the spinal cord. Once these signals reach the brain, it responds by triggering the release of stress hormones such as corticotropin-releasing hormone (CRH), glucocorticoids and epinephrine. While stress impacts the skin mainly through the hypothalamic-pituitary-adrenal (HPA) axis, she adds, the skin also contains a fully functional peripheral HPA system in which CRH, adrenal corticotropin and their receptors are produced in skin cells.
Additional skin stress comes from the release of catecholamines (epinephrine and norepinephrine) through the sympathetic-adrenal-medullary axis, and from the effects of neuropeptides (such as substance P) and neurotrophins (such as prolactin) secreted by peripheral nerves within the skin, says Dr. Schell. Meanwhile, external insults including UV radiation accelerate the skin's natural aging process, producing evidence of chronic low-grade inflammation including coarse and deep wrinkles, mottled hyperpigmentation, sallowness and telangectasias.
Cellular senescence is driven by mechanisms including telomere shortening, genotoxic stress, mitogen stimuli and inflammatory cytokines, all of which can activate the p53 tumor suppressor and/or the cyclin-dependent kinase inhibitor p16, Dr. Schell adds. Clearly, she says, the number of senescent cells, which secrete multiple inflammatory cytokines, in several organs increases with age. "This phenotype of senescent cells is called the senescence-associated secretory phenotype (SASP), which recently has been proposed (in this review) as the main origin of inflammation in both aging and age-related diseases such as atherosclerosis, cancer and diabetes."2
Immunosenescence (age-related dysregulation of the innate immune system) is both characterized by persistent inflammatory responses and accelerated by the presence of chronic inflammatory illness. "Along with cell senescence, dysregulation of immunological imprinting mediated by trained innate immunity might also contribute to persistent low-grade inflammation that occurs even after the initial stimulus has been removed."
Conversely, Dr. Schell says, a recent study has shown that the catecholamines released during exercise may reduce chronic inflammation. In this study, 20 minutes of moderate exercise suppressed monocytic TNF production via B2 androgen receptors.3
Battling cell senescence can be as easy as taking oral supplements, says Dr. Schell. Natural anti-senescence compounds with senolytic effects include tocotrienols, quercetin and piperlongumine.
Natural polyphenols (flavonoids and non-flavonoids) also combat senescence, she says. "We've known about natural polyphenols for a while. That's why people juice. It's probably better to eat the vegetable or fruit, instead of just doing the juicing, and get the cellulose with it. People don't eat a lot of fruit and vegetables anymore." Additionally, synthetic compounds including dasatinib, navitoclax, panobinostat, Hsp90 inhibitors, FOXO4-p53 targeting peptide and 2-deoxy-D-glucose also provide senolytic activity.
To combat the SASP, Dr. Schell says, natural options range from curcumin to catechins, genistein and resveratrol. Synthetic SASP fighters include metformin, rapamycin, JAK inhibitors and aspirin.
Presently, says Dr. Schell, researchers' knowledge of how to counter chronic low-grade inflammation continues to evolve. "We don't really know the correct pathways or how it's going to work. Right now everything is just a big open-minded experiment for people who are interested in this topic." Yet the necessity of reducing chronic low-grade inflammation could hardly be clearer, she says.
Disclosures:
Dr. Schell reports no relevant financial interests.
References:
- Salazar N, Valdés-varela L, González S, Gueimonde M, De los reyes-gavilán CG. Nutrition and the gut microbiome in the elderly. Gut Microbes. 2017;8(2):82-97.
- Sanada F, Taniyama Y, Muratsu J, et al. Source of Chronic Inflammation in Aging. Front Cardiovasc Med. 2018;5:12.
- Dimitrov S, Hulteng E, Hong S. Inflammation and exercise: Inhibition of monocytic intracellular TNF production by acute exercise via β-adrenergic activation. Brain Behav Immun. 2017;61:60-68.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.