- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Oral Vitamin D Supplementation May Lower Melanoma Risk
Author(s):
Researchers were unable to determine a definite correlation.
Pixel-Shot/AdobeStock

A recent study published in Melanoma Research found fewer cases of melanoma among regular users of oral vitamin D supplements than nonusers.1 The study included 498 individuals at risk of any type of skin cancer visiting a dermatology clinic in Finland.
Not surprised by the findings, Kim Margolin, MD, a medical oncologist and the medical director of Saint John’s Cancer Institute Melanoma Program at Providence Saint John’s Health Center in Santa Monica, California, said, “There is definitely something in the vitamin D story versus malignancy. It just needs validation in tightly controlled, randomized, prospective studies, which are very difficult to design and conduct.”
According to the Skin Cancer Foundation, more than 9500 people in the United States are diagnosed daily with skin cancer, and more than 2 people die as a result of the disease every hour.2 Several studies have investigated the role of vitamin D, a UV-B–derived hormone with anticarcinogenic properties, in the prevention and treatment of skin cancers. One such study published in the International Journal of Cancer found higher levels of vitamin D to be associated with a high incidence of several cancers, including melanoma and nonmelanoma skin cancers.3
Vitamin D plays a crucial role in the normal functioning of the human body. Preclinical animal studies have shown that vitamin D alters cancer cell differentiation, proliferation, and apoptosis, making it a candidate agent for cancer regulation. The role of vitamin D in cutaneous carcinogenesis is most likely related to its effects on the regulation of growth, cell death, angiogenesis, and cell differentiation.4 According to an author of this latest study on vitamin D, Ilkka T. Harvima, MD, PhD, a professor in the Department of Dermatology at University of Eastern Finland School of Medicine, “Vitamin D and its metabolites can modulate the cutaneous immune system [and] prevent skin [damage] due to UV light–induced oxidative stress.”
Compared with previous studies, this recent study took a different approach and recruited nearly 500 patients at risk of any type of skin cancer visiting a dermatology clinic. The researchers categorized the patients into 3 groups based on their self-reported use of oral vitamin D (nonuse, occasional use, or regular use) and then divided patients into risk classes for skin cancer (low, moderate, or high risk). Multiple risk factors were taken into consideration, such as past or present premalignant or malignant skin lesions, the severity of skin photodamage, number of moles or atypical moles, Fitzpatrick skin type, immunosuppression, and family history of melanoma.
Margolin commented on the strengths of the study. “It is probably bigger and does attempt to divide the patients into 3 realistic categories—no vitamin D supplementation, occasional, and regular vitamin D supplementation,” she said. “There are probably important differences between taking vitamin D regularly and having levels of vitamin D in the blood (and maybe tissues) that effectively mediate an antioncogenesis effect.”
The findings revealed that compared with nonusers, regular users of oral vitamin D had fewer cases of past or present melanoma and any type of skin cancer. Furthermore, the investigator-estimated risk class of skin cancers was significantly lower among regular users. Logistic regression analysis indicated regular use of oral vitamin D supplements as an independent protective factor of melanoma.1
“This is a cross-sectional study on the first recruitment visit of follow-up patients. Therefore, the causality between vitamin D and melanoma cannot be confirmed by the present study,” Harvima noted, adding that, “Vitamin D alone cannot be considered...an effective medication for preventing or treating melanoma because this skin cancer is very complex in nature. In addition, individual variation can be present.”
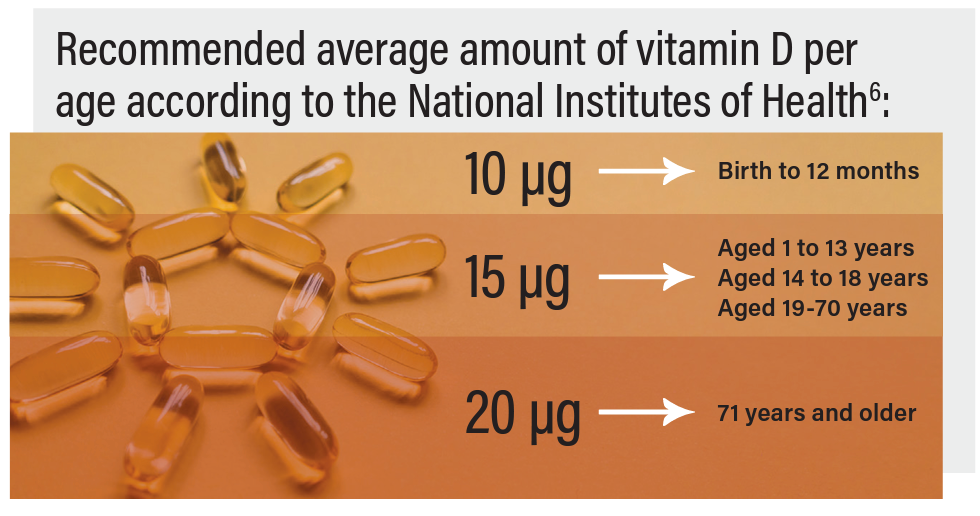
Although several previously studies have demonstrated the beneficial effects of vitamin D against skin cancers, the optimum dose of vitamin D required to reduce cancer risk is yet to be confirmed.6 Hence, it is recommended to use vitamin D according to the national recommendations set in each country.1
“In countries with short daylight in winter, like Finland, one might consider a higher dose, such as 20 to 50 µg a day. However, the dose should not exceed 100 µg a day because of the possibility of toxicity,” Harvima said. “The Finnish Food Authority recommends vitamin D supplementation for adults [older than 75 years], but it is not specifically recommended for people after skin cancer. However, [patients with skin cancer] are instructed to take careful sun protection measures, and consequently, [that] may lead to vitamin D supplementation in response to decreased sun exposure.”
Harvima further noted, “One weakness is that the study cohort does not represent the general population because the [participants] were recruited at the university hospital policlinic based on their risk for skin cancers. Also, it is noteworthy that the cohort size is small for epidemiological studies, vitamin D dose could not be defined reliably, and the self-reported vitamin D supplementation may be biased.”
References
1. Kanasuo E, Siiskonen H, Haimakainen S, Komulainen J, Harvima IT. Regular use of vitamin D supplement is associated with fewer melanoma cases compared to non-use: a cross-sectional study in 498 adult subjects at risk of skin cancers. Melanoma Res. Published online December 28, 2022. doi:10.1097/CMR.0000000000000870
2. Skin cancer facts & statistics. Skin Cancer Foundation. Updated January 2023. Accessed February 2, 2023. https://www.skincancer.org/skin-cancer-information/skin-cancer-facts/
3. Vojdeman FJ, Madsen CM, Frederiksen K, et al. Vitamin D levels and cancer incidence in 217,244 individuals from primary health care in Denmark. Int J Cancer. 2019;145(2):338-346. doi:10.1002/ijc.32105
4. Martin-Gorgojo A, Gilaberte Y, Nagore E. Vitamin D and skin cancer: an epidemiological, patient-centered update and review. Nutrients. 2021;13(12):4292. doi:10.3390/nu13124292
5. van der Pols JC, Russell A, Bauer U, et al. Vitamin D status and skin cancer risk independent of time outdoors: 11-year prospective study in an Australian community. J Invest Dermatol. 2013 Mar;133(3):637-641. doi: 10.1038/jid.2012.346.
6. Vitamin D. National Institutes of Health Office of Dietary Supplements. Updated November 8, 2022. Accessed February 6, 2023. https://ods.od.nih.gov/factsheets/VitaminD-Consumer/

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.





























