- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Sarecycline’s Lipophilicity May Explain Lower Rates of Adverse Events
Author(s):
Study investigators evaluated the blood-brain barrier penetrance and lipophilicity of the narrow-spectrum, third-generation tetracycline-class oral antibiotic used for acne treatment.
Ocskay Bence/AdobeStock

In a recent study published in Frontiers in Medicine1, authors Ayman Grada, MD, MS, Christopher Bunick, MD, PhD, and colleagues analyzed the blood-brain barrier penetration and lipophilic attributes of sarecycline compared with minocycline and doxycycline for the treatment of acne vulgaris. The authors found that sarecycline was not detected in brain samples of rats post dosing and demonstrated a lower lipophilicity profile. “The reduced blood-brain penetrance and lipophilicity of sarecycline compared with other tetracyclines may explain low rates of vestibular-related adverse events seen in clinical trials,” the investigators noted in their discussion.
“The chemistry of the drugs we treat our patients with matters,” Bunick told Dermatology Times®. “The chemical groups on dermatologic medicines have a profound impact on their efficacy, as well as how they interact with the body to potentially cause adverse events. The study demonstrates this concept well with tetracyclines, and how altering a chemical group leads to property changes like lipophilicity, which then affects blood-brain barrier penetrance, which consequently affects real-world symptoms a patient might experience during therapy. It is a great example of translational chemistry going from bench to bedside.”
Overview of Tetracycline-Class Drugs
Minocycline and doxycycline are second-generation tetracycline-class antibiotics that have been used to treat moderate to severe acne vulgaris for decades. Minocycline, however, is often associated with vestibular adverse events such as dizziness and tinnitus, earning itself a central nervous system adverse event warning in the package insert.2 According to Grada et al,1 the adverse effects of minocycline may negatively affect a patient’s ability to complete daily tasks such as driving. The current study found that the higher lipophilicity of minocycline compared with doxycycline allows for higher blood-brain barrier penetration, increasing the risk of dizziness and vertigo.
In contrast, sarecycline is a narrow-spectrum, third-generation tetracycline-class oral antibiotic approved by the US Food and Drug Administration (FDA) in 2018 for the treatment of moderate to severe acne vulgaris. Sarecycline’s safety and efficacy was studied in 2 phase 3 randomized control trials, SC1401 (NCT02320149) and SC1402 (NCT02322866). Results from both trials demonstrated low rates of vestibular-related adverse events, such as dizziness and motion sickness, with no reported events of vertigo or tinnitus, according to Grada et al.
According to the authors, there have been no head-to-head clinical trials comparing sarecycline with other tetracycline-class drugs, limiting the ability to make direct safety and tolerability comparisons. Due to this lack of comparative clinical trials, it remains unclear if the biochemical properties of sarecycline, such as blood-brain barrier penetrance and lipophilicity, could be associated with low rates of vestibular adverse events.
In their study, Grada, adjunct professor of dermatology at Case Western Reserve University School of Medicine in Cleveland, Ohio, Bunick, a physician-scientist, associate professor of dermatology at Yale School of Medicine, dermatologist at Yale Dermatology Associates in Middlebury, Connecticut, and a member of the Dermatology Times® Editorial Advisory Board, and colleagues investigated the potential relationship between the brain-penetrative and lipophilic attributes of sarecycline in 2 preclinical in vivo and in vitro analyses. The first analysis examined the ability of sarecycline to penetrate the blood-brain barrier vs minocycline in a rat model study. The second analysis looked at the lipophilicity of sarecycline compared with minocycline and doxycycline using octanol/water and chloroform/water distribution coefficients (logD).1
Blood-Brain Barrier Study
The blood-brain barrier penetration study used 6 male Wistar rats kept in individual cages with water and feed without restriction and alternating 12-hour light cycles. Following an overnight (about 16 hours) fast, the rats were weighed to determine the appropriate dose volume. Intravenous sarecycline (n = 3) or minocycline (n = 3) at a total dosage of 1.0 mg/kg were delivered to the rats, and food access was restored 2 hours later. After euthanization, brain samples and whole blood were collected from 2 rats at each 1, 3, and 6 hour time points after dosing.1
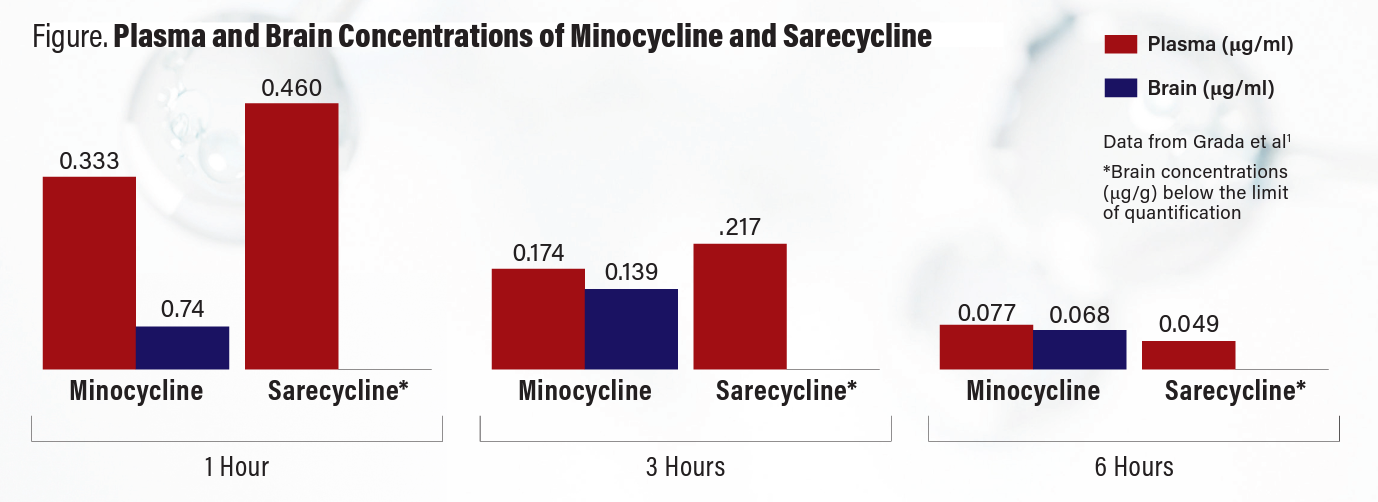
The primary end point of the study was “concentration of sarecycline or minocycline in plasma (μg/ml) and in brain samples (μg/g) at 1, 3, and 6 [hours] post dosing.”1
Although Grada et al found similar concentrations of both agents at each measured hour in the rat plasma, brain samples showed a distinct difference. In the brain samples, the investigators noted sarecycline levels remained below the lower limit of quantitation (0.05 μg/g) at each measured hour, but they found measurable minocycline concentrations at each time point (Figure).
Exploring Lipophilicity
In the lipophilicity study, the authors prepared sarecycline, minocycline, and doxycycline as individual 1.0 mg/ml stock solutions in aqueous-phase pH buffers of 3.5, 5.5, and 7.4. The solutions were quantified by high-performance liquid chromatography prior to mixing with the organic phase and then combined with 2 ml each of aqueous-octanol/chloroform. Final pH values of the aqueous phases were recorded after 24 hours of equilibration and phase separation.
The end point of the study was “the calculation of logD values for each compound at pH 3.4, 5.5, and 7.4.” LogD values were determined using the ratio of the peaks found in the aqueous phase compared with the organic layer. Lower values indicated less lipophilicity, and higher values indicated greater lipophilicity.1
Compared with minocycline in the octanol and water solution, the investigators found sarecycline was less lipophilic at pH 5.5 and 7.4 and more lipophilic at pH 3.5, while doxycycline was in between both agents at the same pH. Interestingly, there was more diversity in results in the chloroform and water solution; compared with minocycline, sarecycline was less lipophilic at pH 7.4, similarly lipophilic at pH 5.5, and more lipophilic at pH 3.5. Grada et al noted that, overall, absolute values of logD were higher in the chloroform/water system than the octanol/water system for sarecycline and minocycline compared with almost no difference in doxycycline logD values recorded between the 2 solvent systems for each pH solution.
Practical Implications
After the study authors performed the 2 analyses of blood-brain barrier penetrance and lipophilicity of sarecycline compared with minocycline and doxycycline, the data showed minocycline was detectable in the brain of the rats and sarecycline was not. In addition, the investigators found that sarecycline had slightly lower logD values compared with doxycycline and minocycline at pH 5.5 and 7.4 in the octanol/water system. The combined results of the study suggest the lower lipophilicity and reduced blood-brain barrier penetrance of sarecycline compared with minocycline may explain the lower incidence of vestibular events (ie, dizziness, tinnitus, and vertigo) seen in sarecycline clinical trials compared with minocycline clinical trials.
Grada et al noted that a possible limitation of the blood-brain barrier penetrance animal study is the small sample size. “However, the trend seen in the results supports previous reports that minocycline has high lipid solubility [and,] thus, may more readily cross the blood-brain barrier compared with other tetracyclines,” the authors wrote.
The study authors noted that no human studies have confirmed the association between higher brain penetrance of minocycline and higher rates of vestibular-related adverse events compared with other tetracyclines. There is also the notable consideration that previously published logD values of tetracyclines, specifically minocycline, are inconsistent across dermatologic literature, according to Grada et al. Previous studies reported that minocycline was 4-fold more lipophilic than doxycycline and 10-fold more lipophilic than tetracycline at a pH of 5.5.3,4 Another study reported that the logD values of minocycline and doxycycline were similar at pH 5.5.5
“Although high drug lipophilicity in the skin is a desirable attribute that helps it to penetrate and accumulate in the lipid-rich pilosebaceous unit, the greater likelihood of crossing the blood-brain barrier in comparison to other tetracycline-class drugs has been attributed to minocycline’s higher lipophilicity. Because of its ability to penetrate the blood-brain barrier, systemic minocycline use in acne treatment has been associated with a relatively higher incidence of vestibular side effects, such as dizziness and vertigo,” Grada told Dermatology Times®.
According to Grada et al, the lower lipophilicity and decreased blood-brain barrier penetration of sarecycline is explained by the chemical structure difference between it and minocycline and doxycycline. The authors noted that all 3 drugs have a common naphthacene 4-ring core, but sarecycline is unique with a long C7 extension that provides improved ribosomal binding through messenger RNA contact. The C7 moiety holds an oxygen atom that acts as an acceptor of hydrogen bonds, reducing lipophilicity.
Grada et al noted that more studies are needed to investigate how sarecycline is related to lower rates of vestibular adverse events compared to other tetracyclines, but the chemical structure suggests the C7 moiety oxygen.1
“I think the information learned here is very practical for real world care of patients prone to vestibular disturbance-related adverse events. Clinicians can now engage in meaningful discussions with patients about history and risk of adverse events related to medications crossing the blood-brain barrier, and where appropriate, explain why sarecycline might be the best choice of oral antibiotic to reduce risk of those adverse events. Ultimately, having a narrow-spectrum antibiotic that does not cross the blood-brain barrier provides additional safety to patients while offering enhanced antibiotic stewardship,” Bunick concluded.
Disclosure
This Grada et al study1 received funding from Almirall, LLC. For a full list of author disclosures, please visit the original publication.
References
1. Grada A, Del Rosso JQ, Moore AY, et al. Reduced blood-brain barrier penetration of acne vulgaris antibiotic sarecycline compared to minocycline corresponds with lower lipophilicity. Front Med (Lausanne). 2022;9:1033989. doi:10.3389/fmed.2022.1033980
2. Solodyn. Prescribing Information. Medicis; Revised March 2011. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/050808s014lbl.pdf
3. Cunha BA, Garabedian-Ruffalo SM. Tetracyclines in urology: current concepts. Urology. 1990;36(6):548-556. doi:10.1016/0090-4295(90)80201-w
4. Leyden JJ, Del Rosso JQ. Oral antibiotic therapy for acne vulgaris: pharmacokinetic and pharmacodynamic perspectives. J Clin Aesthet Dermatol. 2011;4(2):40-47.
5. Colaizzi JL, Klink PR. pH-Partition behavior of tetracyclines. J Pharm Sci. 1969;58(10):1184-1189. doi:10.1002/jps.2600581003

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.
























