- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
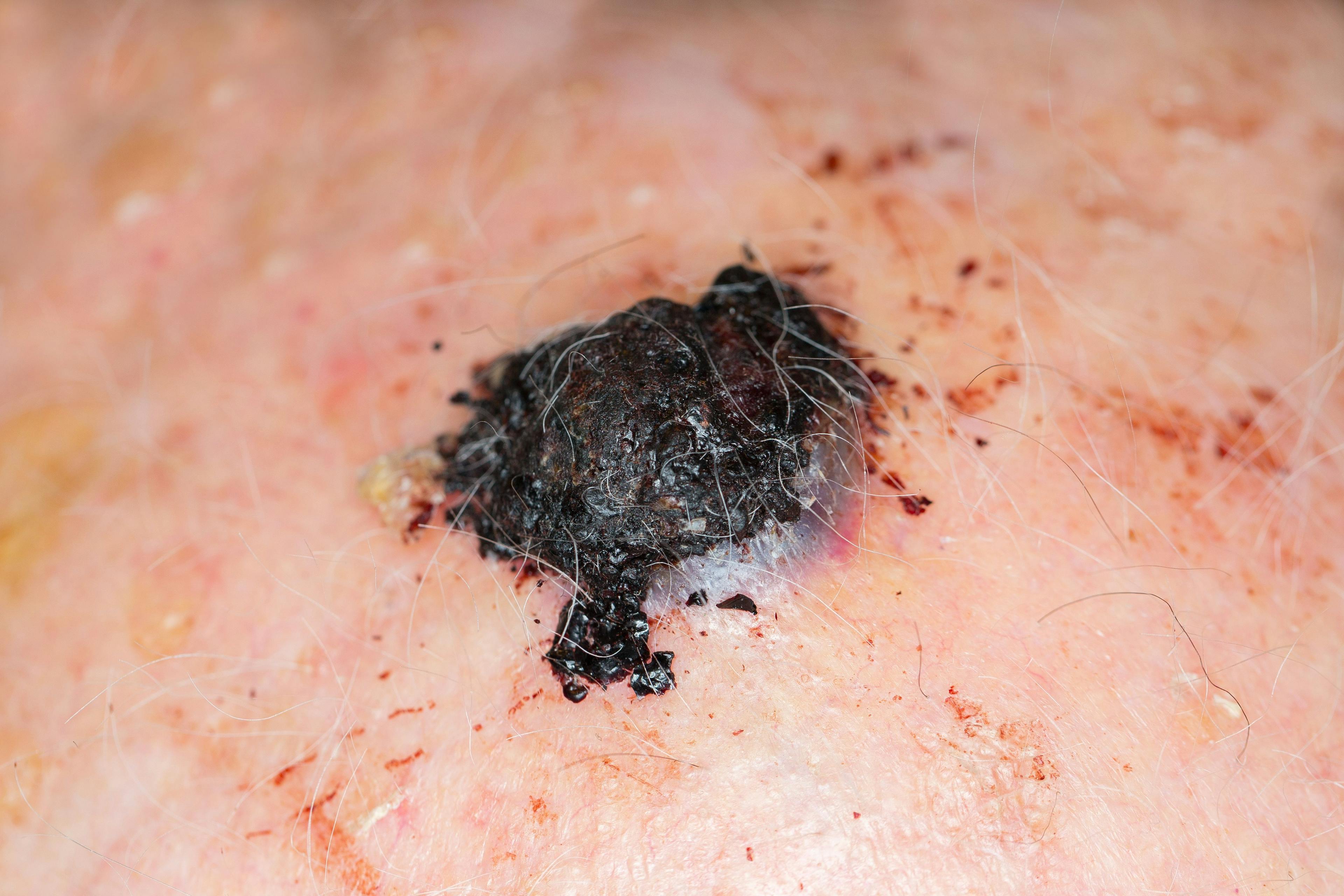
Utility of PRAME staining in identifying malignant transformation of melanocytic nevi
Author(s):
Recently, PRAME (preferentially expressed antigen in melanoma) immunohistochemical staining has shown its usefulness in distinguishing benign from malignant melanocytic cell populations, offering another color to the canvas in the quest for a more definitive diagnosis of melanoma.
Continued research in skin cancer diagnostics has led to advancements in immunohistochemical staining techniques such as PRAME (preferentially expressed antigen in melanoma) that can help clinicians differentiate between benign and malignant melanocytic populations. A recent study found the novel technique to be very useful in distinguishing melanocyte populations of melanoma arising within nevi, helping to identify nevi undergoing malignant transformation and allowing clinicians to better screen for suspicious melanocytic lesions in their patients.
There are several techniques that clinicians have at their disposal to help them more accurately diagnose melanoma and differentiate this skin cancer from benign melanocytic lesions. PRAME is a cancer testis antigen normally expressed in gonadal tissue, and preferentially overexpressed in human melanomas. The diagnostic potential of this encoded protein is still unfolding (it is already utilized in gene expression profiling tests), and it may be used as an adjunctive diagnostic tool to supplement other modalities currently employed to differentiate among lesions that may be undergoing malignant transformation.
“PRAME is a very technically difficult stain to do; its role is not to replace H&E staining. Similarly, with other melanocytic histological staining techniques, PRAME is a diagnostic tool that can help clinicians differentiate between benign and malignant melanocytic cell populations and may push the needle either towards or away from a diagnosis of melanoma,” says Mary E. Lohman, MD, resident dermatologist, Department of Dermatology, USCF, San Francisco, Calif., and head-author of the study.
Dr. Lohman and fellow colleagues recently conducted a study to evaluate PRAME expression in nevus associated melanoma lesions. In the study, all cases of melanoma and melanoma in-situ arising within a nevus over the past five years were identified from the UCSF dermatopathology database. Each case was submitted for PRAME staining and similar to prior studies, PRAME expression was graded 0-4 based on the percentage of labeled cells for each population of melanocytes, both benign and malignant. No labeling was graded 0, 1-25% labeling was 1+, 26-50% was 2+, 51-75% was 3+, and >76% was 4+. No staining at all or grade 0 was indicated as ‘negative’, with grade 1+ to 3+ as ‘intermediate’, and grade 4+ as ‘positive’.
A total of 36 melanomas were identified from the database and were included in the evaluation. Results showed that 67% (24/36) of melanomas were PRAME positive (4+), consistent with previously reported data, while no (0/36) nevi showed 4+ positivity. In addition, 81% (29/36) of nevi were completely PRAME negative compared to 17% (6/36) of melanomas. In 69% of cases (25/36), PRAME differentiated between benign and malignant melanocyte populations. A high rate of differential PRAME staining was observed in adjacent benign and malignant melanocyte populations, while only 2 cases demonstrated identical intermediate PRAME staining for both benign and malignant populations. In PRAME positive melanomas alone, PRAME staining differentiated all benign and malignant melanocyte populations.
“The differential density of staining in the malignant and benign components of a single lesion suggests that whatever is driving PRAME overexpression in malignant melanocytes is likely a late-stage development in the degenerative process. In other words when the burden of mutations reaches a tipping point, and a benign melanocyte starts behaving like a malignant melanocyte, this is when we see melanocytes start to over-express PRAME,” says Aaron Steen, MD, Department of Dermatology, Mayo Clinic, Rochester, Minn., and co-author of the study.
In addition to PRAME having potential future utility in the assessment of margins following wide local excision, Dr. Steen says that PRAME might also be proven useful in the assessment of frozen sections such as during micrographic surgery of melanomas on chronically sun-damaged skin.
“It is important to exercise caution when utilizing a new stain because I don’t think PRAME is going to be the ultimate arbiter of truth between benign and malignant lesions. We know there are other benign lesions that overexpress PRAME such as Spitz nevi and actinic keratoses and as such, clinicians should not rely on this stain alone in the diagnostic workup of suspicious lesions. However, it is an additional tool in the toolbox for the diagnostic workup of suspicious lesions, helping to differentiate between benign and malignant melanocytic neoplasms,” says Dr. Steen.

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.