- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
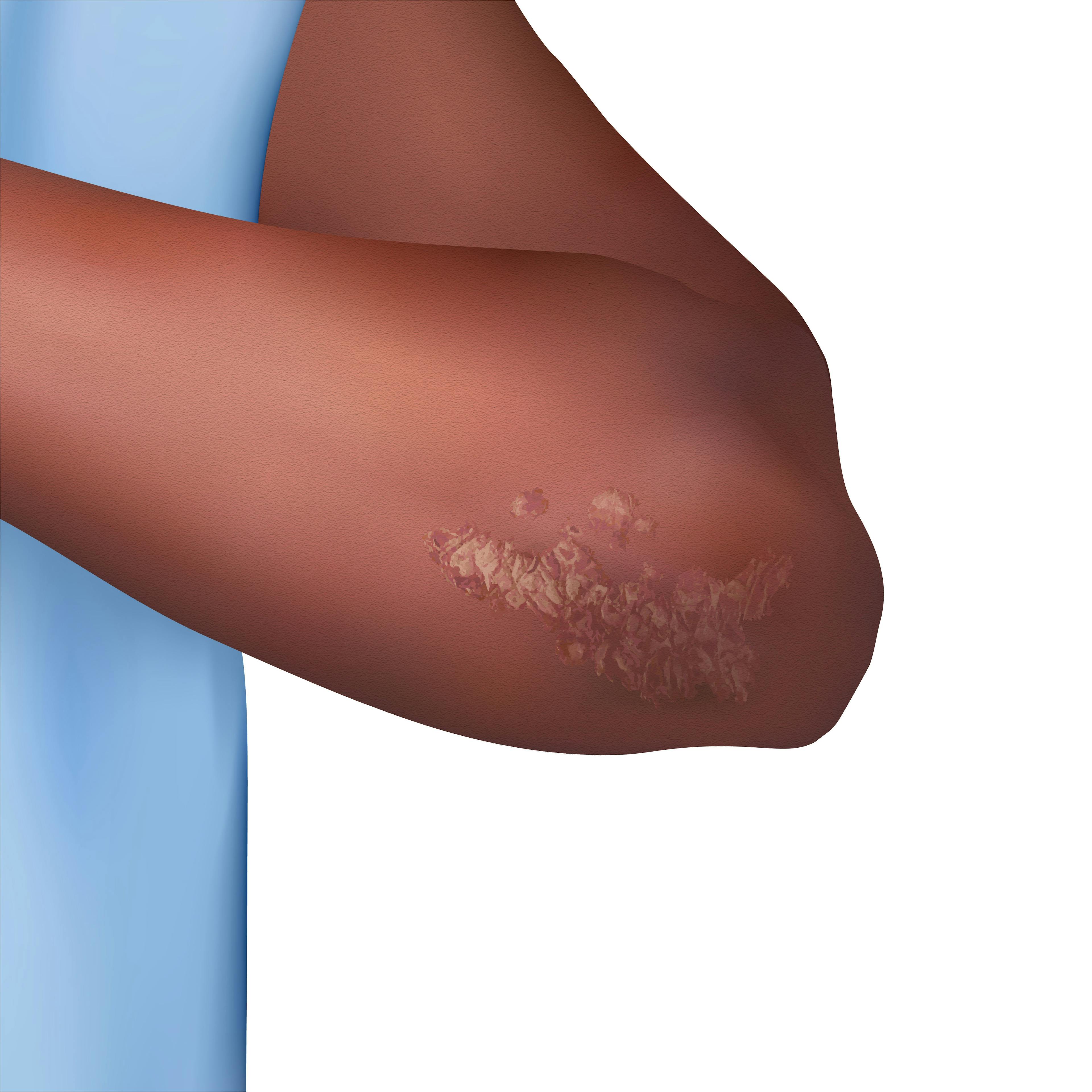
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
1 in 3 Dermatologists Do Not Counsel Patients With HS on Wound Care
Author(s):
Furthermore, a survey showed that more than half of providers do not discuss clothing modifications, and half report providing patients with wound care supplies that are covered by insurance.
As many as 1 third of surveyed dermatologists reported that they do not counsel their patients with hidradenitis suppurativa (HS) on wound care.
Marcin/AdobeStock

In one study,1 researchers sought to evaluate the frequency and importance of wound care counseling or wound care product recommendations for patients with HS. They noted that wound care is an unmet need of the condition due to the presence of acute flares and chronic, draining wounds.
Researchers distributed an anonymous online questionnaire via an email listserv to board-certified and actively practicing dermatologists located in the United States between August and October 2022. The questionnaire consisted of multiple choice questions related to HS, wound care, at-home management, clothing modifications, and more.
In total, 50 dermatologists completed the questionnaire in its entirety. Of these, 38% self-identified as experts in HS.
When asked about their current counseling practices for patients with HS, 90% of dermatologists agreed that patients with HS are in need of greater education surrounding wounds and wound care methods. Furthermore, 70% believe patients with HS lack education of wound care best practices.
Despite this, just over 1 in 4 surveyed dermatologists do not counsel their patients about managing acute flares at home. Even still, more than half (n=52%) reported that they do not counsel patients about clothing modifications, and nearly 1 in 3 said they do not discuss wound care dressings with their HS patients. Exactly half of respondents (n=25) said they order wound care supplies for their HS patients that are covered by insurance agencies.
Additionally, researchers examined dermatologists’ perceptions of the efficacy of several topical agents, including bleach baths, warm compresses, and more.
Of the surveyed dermatologists, the most commonly recommended dresses were abdominal pads, gauze, and panty liners/menstrual pads, while the most highly-recommended at-home methods of management included use of warm compresses, bleach baths, zinc oxide cream, Epsom salt baths, and Vicks VapoRub.
Of these recommended dressings and management tools, dermatologists ranked use of warm compresses, bleach baths, and Epsom salt baths as the most highly effective management tools for HS patients, according to perceived efficacy.
Potential study limitations include a low sample size and proportion of nonacademic dermatologists.
“There are numerous wound care supply companies across the United States that will distribute supplies to patients that are partly or completely covered by insurance. Typically, these orders require documentation of wound size and location in the clinical note and specific requests for supplies... Referrals to wound care can also be beneficial in increasing patient access to wound care supplies. Having access to a variety of dressings has been shown to improve patient quality of life by reducing pain, odor, and staining of clothes,” according to Poondru et al. “These findings underscore areas for improvement in wound care education for patients with HS.”
Reference
- Poondru S, Scott K, Riley JM. Wound care counseling of patients with hidradenitis suppurativa: perspectives of dermatologists. Int J Womens Dermatol. 2023;9(3):e096. Published 2023 Jul 18. doi:10.1097/JW9.0000000000000096
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.