- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
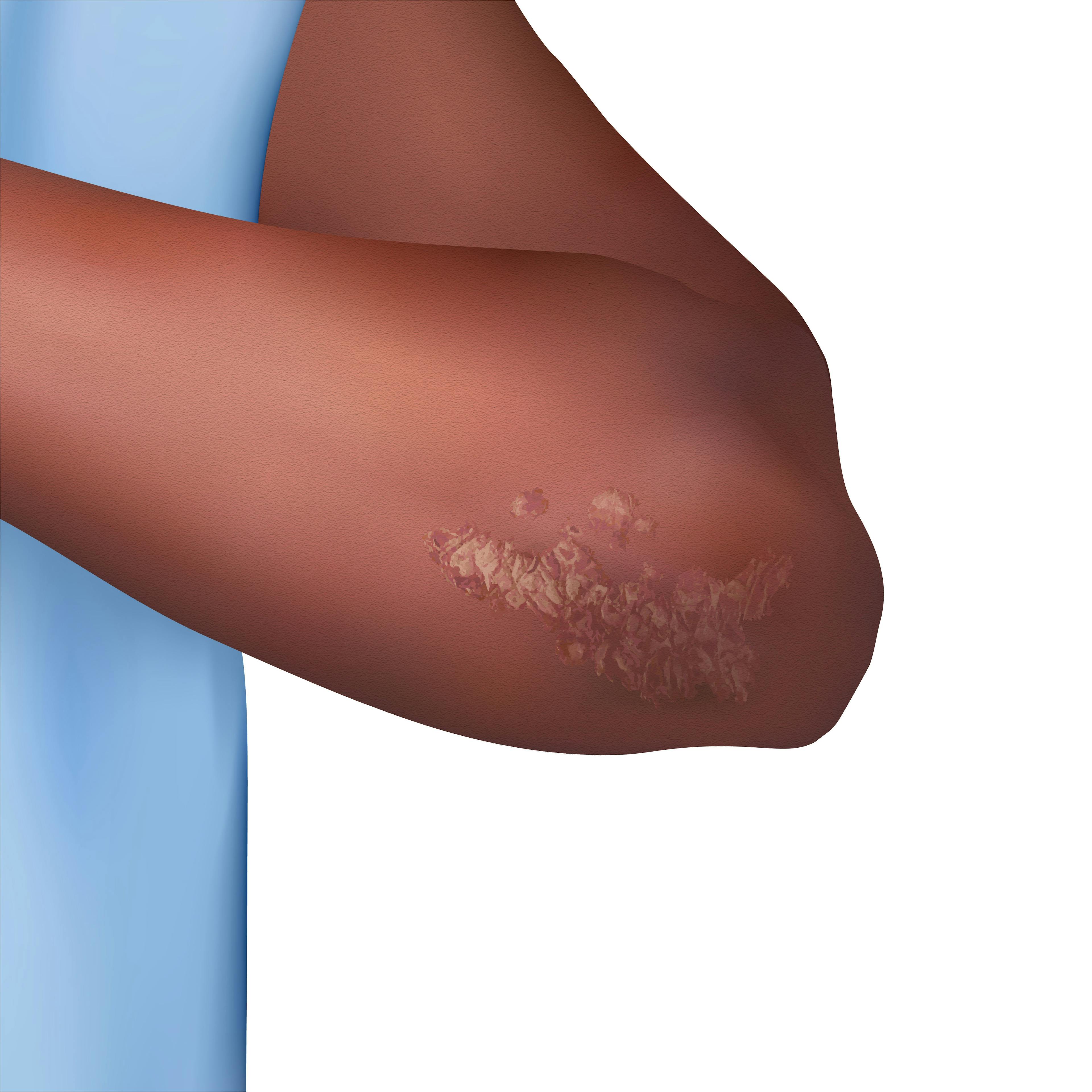
Accurately Recognizing and Diagnosing Psoriasis in Patients With Skin of Color
Author(s):
There may be delays in diagnosis and treatment of psoriasis in patients with darker skin tones due to the clinical presentation variations and less visible erythema.
Nicole A. Negbenebor, MD

Patients of all diverse ethnic backgrounds are affected by psoriasis. There may be delays in diagnosis and treatment of psoriasis in patients with darker skin tones due to the clinical presentation variations and less visible erythema. Some features of psoriasis in darker skin types may also be mistaken for other papulosquamous disorders because they share similar characteristics. Research shows that patients with undiagnosed psoriasis are more likely to have skin of color.1 This article provides a practical checklist to help guide health care professionals in accurately identifying and diagnosing psoriasis in patients with skin of color.
Clinical variations include the following:
- Patients may have increased postinflammatory hyperpigmentation or hypopigmentation in areas of previous skin involvement. These patches and macules of dyspigmentation are due to inflammation altering the production of melanin.2 Depending on the severity and location, these patches and macules may resolve within a few months to a year. Providers should be aware that patients can be most bothered by the dyspigmentation and that this may be the chief complaint rather than one about the psoriasis itself.2,3
- Erythema may be more subtle or appear hyperpigmented, gray, and/or violaceous. This may lead to a lower overall PASI score (Psoriasis Area and Severity Index) since the erythema can present with a darker hue in patients with darker skin tones. Providers need to be aware that the violaceous or hyperpigmented hues can be a sign of ongoing inflammation rather than postinflammatory hyperpigmentation.2-4
- Overlapping papulosquamous conditions that could mimic psoriasis include cutaneous lupus erythematosus, sarcoidosis, cutaneous T-cell lymphoma, pityriasis versicolor, and lichen planus. Patients should have a full body skin examination, including the nails and scalp, to help with diagnosis of psoriasis. A biopsy may be needed for confirmation.5
- Because of delays in care, patients with skin of color may initially present to the clinic with a greater body surface area affected.6
- Scale may be thicker or more severe in patients with hair textures that do not allow for frequent hair washing. Buildup of scale can be more prominent throughout the scalp.7 Research shows that Black and Asian patients are more likely to have scalp psoriasis.7
- Asian and Hispanic patients can present more frequently with pustular psoriasis. Asian patients are also more likely to have inverse psoriasis and develop erythrodermic psoriasis.8,9
In conclusion, it is imperative that health care professionals accurately recognize and diagnose psoriasis in patients with skin of color. This requires a comprehensive understanding of the unique clinical variations that patients can present with for psoriasis. By leveraging this checklist, health care professionals can improve care for patients of diverse racial and ethnic backgrounds. This will provide effective and timely management of psoriasis in patients with skin of color and minimize delays in diagnosis.
Nicole Negbenebor, MD, is a Mohs micrographic surgery and cutaneous oncology fellow in the University of Iowa’s Department of Dermatology.
References
- Kurd SK, Gelfand JM. The prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003-2004. J Am Acad Dermatol. 2009;60(2):218-224. doi:10.1016/j.jaad.2008.09.022
- Alexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007;80(5):387-394.
- McMichael AJ, Vachiramon V, Guzmán-Sánchez DA, Camacho F. Psoriasis in African-Americans: a caregivers’ survey. J Drugs Dermatol. 2012;11(4):478-482.
- Wang CQ, Akalu YT, Suarez-Farinas M, et al. IL-17 and TNF synergistically modulate cytokine expression while suppressing melanogenesis: potential relevance to psoriasis. J Invest Dermatol. 2013;133:2741-2752. doi:10.1038/jid.2013.237
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7(11):16-24.
- Shah SK, Arthur A, Yang YC, Stevens S, Alexis AF. A retrospective study to investigate racial and ethnic variations in the treatment of psoriasis with etanercept. J Drugs Dermatol. 2011;10(8):866-872.
- Kaufman BP, Alexis AF. Psoriasis in skin of color: insights into the epidemiology, clinical presentation, genetics, quality-of-life impact, and treatment of psoriasis in non-white racial/ethnic groups. Am J Clin Dermatol. 2018;19(3):405-423. doi:10.1007/s40257-017-0332-7
- Yan D, Afifi L, Jeon C, Cordoro KM, Liao W. A cross-sectional study of the distribution of psoriasis subtypes in different ethno-racial groups. Dermatol Online J. 2018;24(7):13030/qt5z21q4k2.
- Sangha AM. Special considerations in the diagnosis and treatment of psoriasis. J Clin Aesthet Dermatol. 2021;14(12 suppl 1):S24-S25.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.