- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
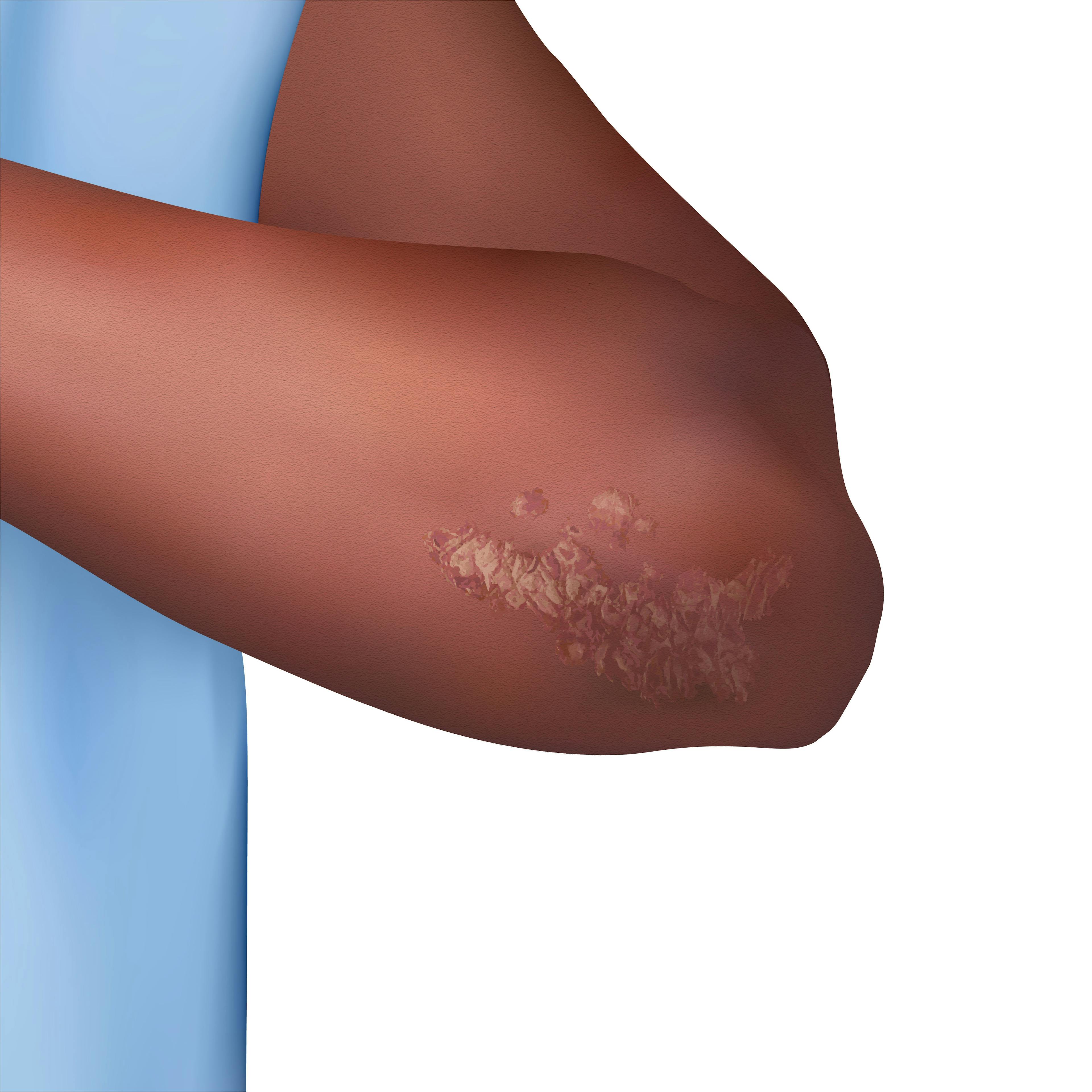
Addressing Cultural Disconnect in Patients With Vitiligo
Author(s):
Clinicians can use culturally competent care to ease patients’ concerns with identity and better understand the emotional toll of the condition.
blackday/Adobe Stock

Among the myriad of challenges faced by patients with the condition is a struggle with personal identity and a sense of disconnect from their own culture as they reconcile with their visibly changing skin.1,2
Omar Noor, MD, FAAD, a board-certified dermatologist who practices in New York and New Jersey, says providing culturally competent care is the key to helping patients who are struggling with their identity.
“Culturally competent care is something that you have to think about when you’re treating patients,” Noor said. He explained various cultures may have specific stigmas or sensitivities, especially with vitiligo, and it is important to be aware of this. “Sometimes you have to make it a point to truly put yourself in the patient’s skin and appreciate where they’re coming from,” he said.
Noor provides dermatology clinicians with pearls and best practices for culturally competent and compassionate care in the management of vitiligo.

Recognize the Effects of the Patient’s Changing Appearance
Although loss of pigment may be more apparent in patients with darker skin types due to a greater contrast, Noor said it is important to recognize that this does not diminish the effect of pigment loss on white patients.
“As we see that in our darker skin types, we have to appreciate its effects not only on the patient, but [in] the way the patient views themselves in the eyes of their friends, their family, the people around them,” he said.
Practice Compassion and Encourage Appreciation
In addition to the stigma3 surrounding vitiligo, patients with ties to certain cultures may face myths and misconceptions centered around their condition. According to a 2022 abstract published in Dermatological Reviews, there are several prevalent myths and misconceptions about vitiligo in vaious regions of the world, including the Middle East and Southeast Asia, including confusing vitiligo with leprosy.2
Noor shared that a patient with vitiligo depigmentation located on the arm once asked whether the arm could be amputated, all because of the stigma.
“That is the impact that vitiligo can have, psychologically, on another human being,” Noor said. “For a lot of these patients, some people even think that it might even be contagious. You have to be very compassionate, and you have to be educational. You want these patients to understand that this is not their fault and that we are learning more about this autoimmune condition that we call vitiligo, and really educating them on why it’s happening and the different tools that we have in order to improve that.”
Offer the Appropriate Mental Health Resources to Your Patients
“The most important thing is to start by educating an individual that’s looking to such an extreme. They may have a different mindset: ‘I have this hidden disease. Maybe it’s contagious. I can’t hold my children; I’m going to give it to them by touching them.’ Educating around what they have, and how we have tools to help repigment the skin. Once they can appreciate that, they can appreciate that it’s going to take time, but we’re going to move in a positive direction,” Noor said.
Due to the psychological effects of vitiligo,1 Noor believes ensuring patient access to appropriate mental health care and resources is important. “Whether it’s a psychiatrist or primary care doctor, making sure that they have the appropriate network around them so that not only do they understand, but their family understands, their friends understand, what they’re dealing with, what they’re treating, and then we can all work together towards a resolution,” he said.
Be Mindful When Balancing Appreciation and Offering Treatment Perspectives
“Vitiligo is especially challenging, mostly because we only recently have our first FDA-approved option for treatment,4 and our treatment options have been limited previously,” Noor said.
“But the other major, challenging component for vitiligo is the fact that we have patients in dermatology, in skin diseases, whether it’s acne, psoriasis, atopic dermatitis, everything that we talk about and we do: ‘I want to get you better, and I want to get you better faster.’ With vitiligo, that is not the case. It’s just not the way the disease works. We have to be patient, and we have to make sure that our patients are patient because the repigmentation takes time. They have to be aware that it’s going to take effort. It’s going to take time, but we’ll get there together.”
Encourage Continued Patient Education to Eliminate Vitiligo Stigma
According to Noor, patient education is the foremost best practice for eliminating vitiligo stigma and providing more compassionate care. “We know that vitiligo is an autoimmune condition. We know that genetics plays a very large role in that, but at its core, vitiligo is an inflammatory condition. Understanding that we can now attack vitiligo with topical JAK inhibition really allows us to address that in our patient,” Noor said.
“Educating around the treatment: It’s going to take time; some areas may read pigment faster than other areas. We’re lucky that areas like the face that have more hair follicles will repigment faster. Areas that have less hair follicles will repigment slower, but we have to have that conversation with the patient so that they can know what to expect going forward. And as we become more educated as providers, then we can then go on to educate our patients more,” concluded Noor.
References
- Grimes PE, Miller MM. Vitiligo: patient stories, self-esteem, and the psychological burden of disease. Int J Womens Dermatol. 2018;4(1):32-37. doi:10.1016/j.ijwd.2017.11.005
- Mehta N, Gupta V. Psychosocial impact of vitiligo in patients with skin of color. Dermatological Reviews. 2022;3(5):269-275. doi:10.1002/der2.148
- Hedayat K, Karbakhsh M, Ghiasi M, et al. Quality of life in patients with vitiligo: a cross-sectional study based on Vitiligo Quality of Life index (VitiQoL). Health Qual Life Outcomes. 2016;14:86. doi:10.1186/s12955-016-0490-y
- FDA approves topical treatment addressing repigmentation in vitiligo patients aged 12 and older. FDA. July 19, 2022. Accessed August 11, 2023. https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-topical-treatment-addressing-repigmentation-vitiligo-patients-aged-12-and-older
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.