Understanding and effectively communicating the value of cutaneous cancer treatments in the setting of a palliative care plan can be tough. Kathryn Schlenker, DO, and professor and associate program director of palliative care at the University of Washington Medical Center Montlake, presented pearls and considerations in determining and communicating a palliative care plan during the session “On the Margin: Reasons to Avoid or Discontinue Mohs Surgery” at the 2023 American College of Mohs Surgery Meeting in Seattle, Washington.1
Palliative care is specialized medical care for people living with a serious illness. It is focused on providing relief from the symptoms and stress of a diagnosis and improving quality of life for both the patient and their familiy.2 It is a common consensus that palliative care is the same thing as hospice. While both consist of symptom management and support, hospice is used when life expectancy is less than 6 months, is oriented toward comfort, and typically takes place in a patient’s home. Palliative care can be used at any point in a serious illness, can be utilized alongside curative treatments, and the location of care varies depending on the patient’s goals. During the presentation, Schlenker shared a bowtie visual introduced by Pippa Hawley, BMED, FRCPC, and head of the palliative care division at the University of British Columbia, that can be helpful in visualizing what a palliative care plan can look like.3
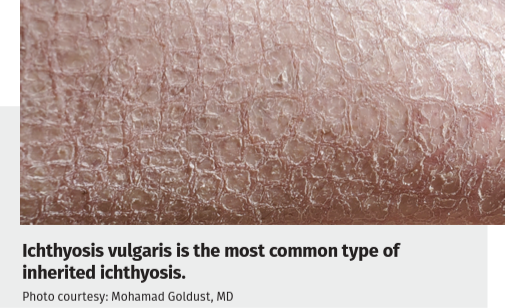
The bow tie model of 21st century palliative care. Courtesy: Canadian Virtual Hospice
As a physician explaining palliative care, the goals are to help a patient determine their goals of care, support them with complex medical decisions, manage symptoms, share insight on advanced care planning options, and provide support for their family with education and referrals to grief or end of life resources. Schlenker pointed out that it is not easy telling a patient Mohs surgery cannot be performed and recommended keeping the acronym REMAP in mind when breaking the news.4
What is REMAP?
Reframe: “We are in a different place.”
Expect emotion and empathize: “I can see how hard this is.”
Map the future: “Given this situation, what is the most important to you?”
Align with patient’s goals and values: “As I listen to you, it seems like the most important things are...”
Plan medical treatments: “Here is what I can do now that will help you do those important things. What do you think about it?”
Throughout palliative care, it is important to check in with the patient in their family periodically with questions such as:
- What is your understanding now of where you are with your illness?
- What are you hoping for?
- What are your concerns or worries?
- What abilities are so critical to your life that you can’t imagine living without them?
- If you become sicker, how much are you willing to go through for the possibility of gaining more time?
- What gives you strength as you think about the future with your illness?
- Do you have any prior experience with serious illness?
Schlenker highly recommends utilizing the website Vital Talk for resources on conversation guides for clinicians. She and the other session’s presenters wrapped up the session with an open, candid discussion on a variety of patient reactions to a serious diagnosis Mohs surgery could not fix. Her concluding thought was to lead with empathy and to not fear silence.
“Allow for silence in these conversations. We spend so much time as physicians talking to patients and don't often allow for silence. There are a couple of studies that show when a patient is first going into the physician's office and explaining what's happening and what their chief complaint is, we give them 11 seconds in 1 study and others that it was up to 23 seconds before we interrupt,” Schlenker explained. “We're so used to giving information and I think these conversations really are a time to slow down and allow for silence. One of my favorite social workers who I've worked with on my palliative care team when I was a fellow helped me retrain my brain and count for 6Mississippis. It was so hard and I'd have to sit there, squeeze my hand, and count.Sometimes when you get to the fourth or fifth Mississippi, the patient opened up and they start saying something, and then they lead us to where we need to be rather than us fumbling and trying to take them there. They get to lead us.”
References
1. Brewer J, Carroll B, Mafee M, Schlenker K. On the margin: reasons to avoid or discontinue Mohs surgery. Presented at: 2023 American College of Mohs Surgery Meeting; May 4-7, 2023; Seattle, WA.
2. Hallenbeck JL. Palliative Care Consults. Palliative Care Perspectives. 2021:210-226. doi:10.1093/med/9780197542910.003.0010
3. Hawley P. The bow tie model of 21st century palliative care. The Bow Tie Model of 21st Century Palliative Care | The Exchange | Canadian Virtual Hospice. Published January 2015. Accessed May 7, 2023. https://www.virtualhospice.ca/en_US/Main+Site+Navigation/Home/For+Professionals/For+Professionals/The+Exchange/Current/The+Bow+Tie+Model+of+21st+Century+Palliative+Care.aspx.
4. Transitions/goals of care. Vital Talk. Published May 9, 2019. Accessed May 7, 2023. http://www.vitaltalk.org/guides/transitionsgoals-of-care/.