- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Current Research Reveals New Treatment Options for Ichthyosis
Author(s):
Research and ongoing clinical trials are giving some hope to those with ichthyosis but for now most people manage their disease symptomatically.
With at least 20 recognized variants of the disease, the large group of heterogeneous genetic skin disorders commonly known as ichthyosis remains very challenging to manage because effective therapies are few and far between. Although it is still early, continued research and ongoing clinical trials are giving some hope to this patient population. However, for the time being, most patients can manage their disease only symptomatically.1
Symptoms and Variants
Whether it is the inherited or acquired form of the disease, ichthyosis is typically characterized by the presentation of scaly skin with varying degrees of scale, thickening, desquamation, and erythema in the affected areas. Depending on the type of ichthyosis, symptoms can vary from mild to severe with potentially life-threatening implications. This family of skin cornification disorders results in defective keratinocyte differentiation and abnormal epidermal barrier function, leading to increased transepidermal water loss and inflammation. Many patients with ichthyosis, regardless of the variant, will often experience various degrees of intense pruritus, excoriations, recurrent infections, hypohidrosis and subsequent heat intolerance, and diverse ocular, hearing, and nutritional complications.
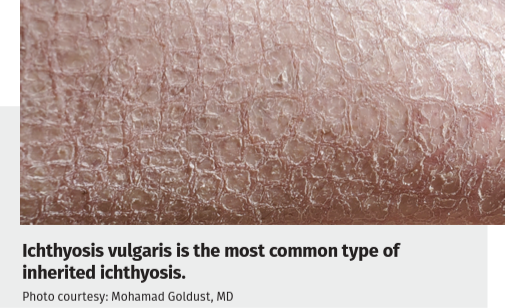
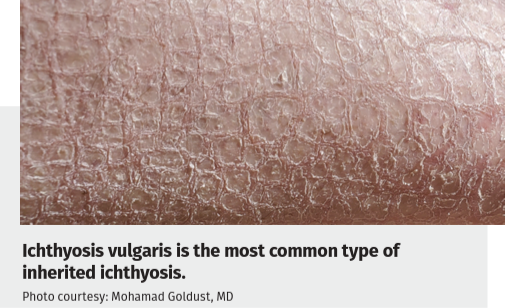
There are many variants of ichthyosis that are classified by their clinical appearance, whether they are syndromic or not, and by the mode of inheritance. Common types of inherited ichthyosis include ichthyosis vulgaris, recessive X-linked ichthyosis, autosomal recessive congenital ichthyosis, and keratinopathic ichthyosis. Acquired ichthyosis tends to develop in adulthood and is usually associated with other conditions including hypothyroidism, renal disease, sarcoidosis, Hodgkin lymphoma, and HIV infection. Ichthyosis vulgaris is the most common type of inherited ichthyosis, affecting approximately 1 in 250 individuals worldwide, and can usually be managed well with topical therapies. The autosomal recessive congenital ichthyoses such as lamellar ichthyosis, congenital ichthyosiform erythroderma, and harlequin ichthyosis are much rarer variants of the disease, with the latter having an overall incidence of approximately 1 in 300,000 newborns and requiring intensive neonatal support and care.
“The inherited and acquired forms of ichthyosis have been well established, and current research is particularly focused on potential therapies that can address this very burdensome and sometimes devastating disease. Fortunately, current treatment options have expanded and become more than just frequent bathing and moisturizing and hydrating the skin with emollients. Currently, there are no FDA-approved treatments for ichthyosis; however, we are hopeful that this may change in the near future,” Mohamad Goldust, MD, said. Goldust is a postdoctoral fellow at Yale School of Medicine in New Haven, Connecticut.
Treatment Options
Traditional mainstay treatment approaches for ichthyosis are focused on hydrating the skin with emollients and moisturizers with the goal of trapping moisture within the skin, which can lead to an amelioration of the presenting dryness and scaling, in addition to using the keratolytic agents. According to Goldust, topical treatments containing various percentages of urea, propylene glycol, lactic acid, and α-hydroxy acids have shown particular usefulness in exfoliating the skin. These topical therapeutic measures work best when applied while the skin is still moist, such as after bathing, and should ideally be applied within 2 minutes of bathing. Environmental humidification can also be a useful therapeutic measure patients can take to help quell symptoms.

Taking frequent and long baths is an important cornerstone of therapy that can help soften and release the excessive scaling typically seen in patients. Patients with ichthyosis will often require antiseptic and topical and/or systemic antibiotics to address the skin infections that can often arise. In those patients with a higher incidence of skin infections, a small amount of bleach can be added to the bath which can help reduce the microbial load on the skin and reduce the frequency of skin infections.
Currently, there are different medications being evaluated in various phases of clinical trials. The retinoids, including topically administered tretinoin, adapalene, and tazarotene as well as systemically administered isotretinoin and acitretin, are key components in the management of most types of ichthyosis. One of the most recent developments in therapy is a topical vitamin A derivative that has shown significant efficacy in helping to quell symptoms.1 According to Goldust, vitamin A derivatives such as isotretinoin, both in the topical and systemic forms, currently appear to be the most effective therapy and the most useful in those patients with lamellar ichthyosis, congenital ichthyosis erythroderma, and harlequin ichthyosis.
“In our experience, vitamin A derivatives appear to be exceedingly effective in most cases of moderate to severe ichthyosis and emollients and keratolytics the most effective in ichthyosis vulgaris, the most common form seen in patients,” Goldust said. In addition, topical delivery of ceramides combined with cholesterol has shown effectiveness in some types of ichthyosis, including recessive X-linked ichthyosis.
Recent Research
Much has been learned recently from clinical experience with biologic therapy for inflammatory skin diseases such as psoriasis. According to Goldust, although novel therapies, including biologic agents, small molecules, enzyme replacement therapies, and genetic therapies, have been proposed, none have had broad use in management of ichthyosis.
Genetic testing is a very important aspect in the diagnostic work-up of ichthyosis to better understand the pathophysiology of the disease and help clinicians arrive at the accurate diagnosis and appropriate management of patients’ skin disorders. An accurate molecular diagnosis is crucial for predicting prognosis and providing appropriate genetic counseling. According to Goldust, clinics and medical centers that provide genetic testing using whole-exome sequencing technology, which can investigate the many different genes responsible for ichthyosis, are paramount and requisite for complete patient care.
“Depending on the type and severity, ichthyosis can be a devastating disease and have a significant physical as well as psychological impact on patients. In addition to providing clinical care, I believe that it is paramount that dermatologists take the time and listen to their patients to help them through their disease. Patients need to be cared for with passion, because their disease can be extremely frustrating for them and their family and loved ones,” Goldust said.
Because there is no definitive cure for ichthyosis, the therapy is lifelong, with the best prognosis seen in the inherited ichthyosis vulgaris variant of the disease. In addition to managing symptoms, consulting physicians and their patients with acquired ichthyosis should focus on addressing the triggers of the disease, which include associated diseases such as lupus erythematosus, renal disease, sarcoidosis, and lymphoma as well as medications such as statins, allopurinol, isoniazid, acitretin, and hydroxyurea. Reducing the dosage of triggering medications can often result in a mitigationof symptoms.
Disclosures: None relevant
Reference
- Bunick CG, Teng JMC, Guenthner S, et al. Characteristics and outcomes for participants with congenital ichthyosis who responded to treatment with the topical isotretinoin formulation TMB-001: results from the phase 2b CONTROL study. Clin Exp Dermatol. Published online March 17, 2023. doi:10.1093/ced/llad105

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.