- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Considerations to Best Serve Transgender Patients Seeking Aesthetic Care
Author(s):
Ronda Farah, MD, and her colleagues reviewed how dermatology providers play an important role in transgender aesthetic care.
Dermatology is occupying an increasingly important role in the provision of gender-affirming care to transgender and gender diverse (TGD) people seeking to align their gender expression and identity. This care can take on a variety of forms, ranging from social and legal affirmation to medical and procedural therapy, including numerous aesthetic and minimally invasive procedures. As of 2022, approximately 1.3 million US adults identify as transgender.1 According to the American Society of Plastic Surgery, over 16,000 gender affirmation surgeries were performed in 2020, nearly 2000 more than the year prior.2 Dermatologists are experts in many of the medical treatments and minimally invasive procedures gender diverse individuals seek. Such procedures include laser hair reduction, laser scar treatment, neurotoxins, soft tissue augmentation, body sculpting and contouring, andalopecia management.
Laser hair removal (LHR) is one of the most common noninvasive procedures sought by transgender patients.3 Patients seeking laser hair removal may be seeking facial, neck, and chest hair removal along with or in preparation for bottom surgery. Bottom surgery, also known as genital reconstruction surgery, involves the surgical alteration of the genitals to match the patient’s gender identity.4 This can include procedures such as vaginoplasty or labiaplasty for transgender women or phalloplasty for transgender men.4 Bottom surgery preparation often involves hair reduction via LHR or electrolysis. Within the field of plastic surgery, intraoperative destruction of the hair follicle may also be used. Patients electing LHR should be counseled on the need for a series of treatments, pain with procedure, and lack of efficacy when used on red, white, or gray hair. Risks of any laser include scarring, dyspigmentation, blistering, and herpetic reaction. Condyloma should be managed in the area prior to LHR. Furthermore, LHR devices are not FDA cleared for bottom surgery preparation. Hair may return in the future, and this can lead to obstruction of the neourethra and hair growth within the neovagina. Understanding the patient’s goal surgical date and coordinating the location of hair removal with the performing surgeons are also key to a successful management plan.
In addition to LHR, the dermatologist may manage the postoperative scarring from top and bottom surgery. Top surgery, also known as chest reconstruction surgery, results in scarring that may be bothersome to the patient. Top surgery involves the removal of breast tissue in transgender men or the creation of a chest contour with the use of implants in transgender women.5 Top scars vary based on the patient and/or surgical technique, but in our experience, they are often periareolar or horizontal and linear. Scar management may include the use of laser-based technologies to manage fish mouthing, hypertrophic scars, and keloids. In our experience, the use of the pulsed dye laser in combination with ablative or nonablative resurfacing devices can be helpful. Furthermore, laser-assisted drug delivery of steroids can assist with hypertrophic scars that do not respond tosteroids alone.
Figure 1. Male-to-Female (MtF) gender affirmation
injectable example. Of note, not all patients are seeking MtF injectables.
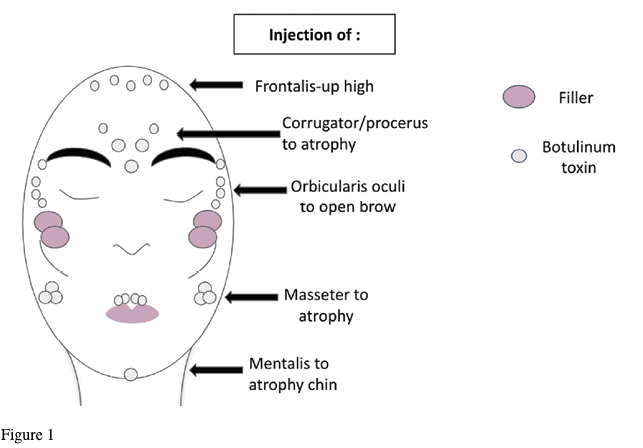
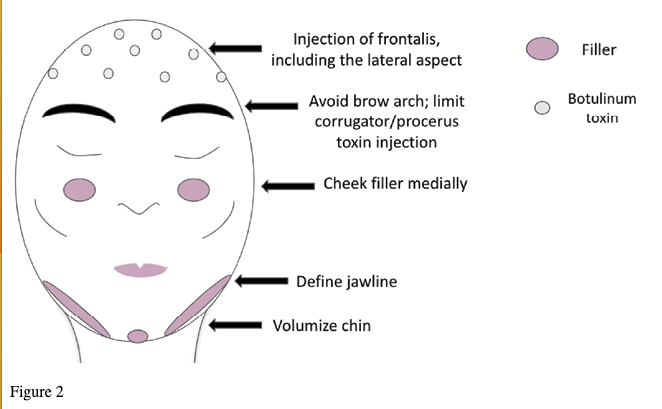
Craniofacial surgery and soft tissue augmentation are also options for individuals seeking to modify their facial appearance as part of gender affirmation. The use of injectables for soft tissue augmentation is appealing to many given the temporary and minimally invasive nature. However, for those patients who desire a surgical craniofacial assessment, neurotoxins and fillers should be deferred as these can prevent adequate pre-surgical planning. Dermatologists should work with their patients to identify which facial characteristics the patient hopes to maintain and which they hope to modify. (Figures 1 and 2)
Figure 2. Female-to-Male (FtM) gender affirmation
injectable example. Of note, not all patients are seeking FtM injectables.
Finally, hairline alteration and management of androgenetic alopecia (AGA) are important considerations. Transgender women may desire advancement of the hairline and increased hair density on the crown. Transgender men commonly experience unwanted AGA as an adverse effect of testosterone therapy, and most desire a greater density of facial and body hair than that achieved with testosterone alone.6–8 Importantly, AGA may not necessarily be seen as an undesirable side effect of testosterone therapy as some transmasculine individuals may embrace it as part of their own unique affirmation goals. On the other hand, some may strongly desire treatment. Patients who are already on spironolactone and finasteride may choose to add photobiomodulation, hair transplantation, platelet-rich plasma, topical minoxidil, or oral minoxidil. Of note, transgender women should be counseled that oral minoxidil can cause unwanted facial hair. Transgender men may find oral minoxidil beneficial in growing scalp, chest, facial, and other body hair. It is important to counsel transgender men with reproductive potential regarding the potential complications of teratogenic medications.
In conclusion, dermatologists are important members of the multidisciplinary gender-affirming care team. Not only is dermatology uniquely equipped to manage complications of hormone therapy, but it also plays a direct and increasingly important role in providing access to aesthetic and minimally invasive procedural options that facilitate the alignment of gender expression with gender identity. Laser hair reduction, laser scar treatment, injectables, and alopecia management are among the many examples of gender-affirming care that dermatologists can support and offer. However, it is important to note that gender-affirming care faces growing legislative restrictions nationwide with almost 20 states as of May 2023 signing legislation into law restricting access to evidence-based care for transgender people. The legislative language is highly variable depending on the state. While dermatology is not explicitly referenced (likely as a result of lack of awareness among legislators of the role of dermatology in gender-affirming care), surgical and procedural care is not clearly defined and in many cases could arguably include many of the minimally invasive procedures performed by dermatologists. Moreover, many states have included prohibitions on simply “aiding or abetting” gender-affirming care, which could further implicate the participation of dermatologists in this care. Numerous lawsuits challenging the legality of these restrictive bans are already underway, and the reality of this landscape moving forward remains unclear for now. In the meantime, advocacy for the rights of transgender people to access evidence-based careis essential.6
Author Bios
Ronda Farah, MD, is a dermatologist and associate professor at the University of Minnesota.
Sophia Fruechte, Nathalie Ly, and Zachary Wendland, MD, are research fellows at the University of Minnesota.
James Pathoulas, MD, is a dermatology resident at Stanford University.
Klint Peebles, MD, is a dermatologist at Mid-Atlantic Permanente Medical Group in Washington, DC.
References
1. How many adults and youth identify as transgender in the United States? Williams Institute. June 2022. Accessed May 19, 2023. https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/
2. Plastic surgery statistics report.Society of Plastic Surgeons. Accessed May 19, 2023. https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf
3. Ginsberg BA. Dermatologic care of the transgender patient. Int J Womens Dermatol. 2016;3(1):65-67. doi:10.1016/j.ijwd.2016.11.007
4. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep. 2018;19(8):62. doi:10.1007/s11934-018-0809-9
5. Ammari T, Sluiter EC, Gast K, Kuzon WM Jr. Female-to-male gender-affirming chest reconstruction surgery. Aesthet Surg J. 2019;39(2):150-163. doi:10.1093/asj/sjy098
6. Shin L, Kole LC, Peebles JK. Legislative efforts restricting care for transgender people. JAMA Dermatology. Published online April 26, 2023. doi:10.1001/jamadermatol.2023.0771

Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.