- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
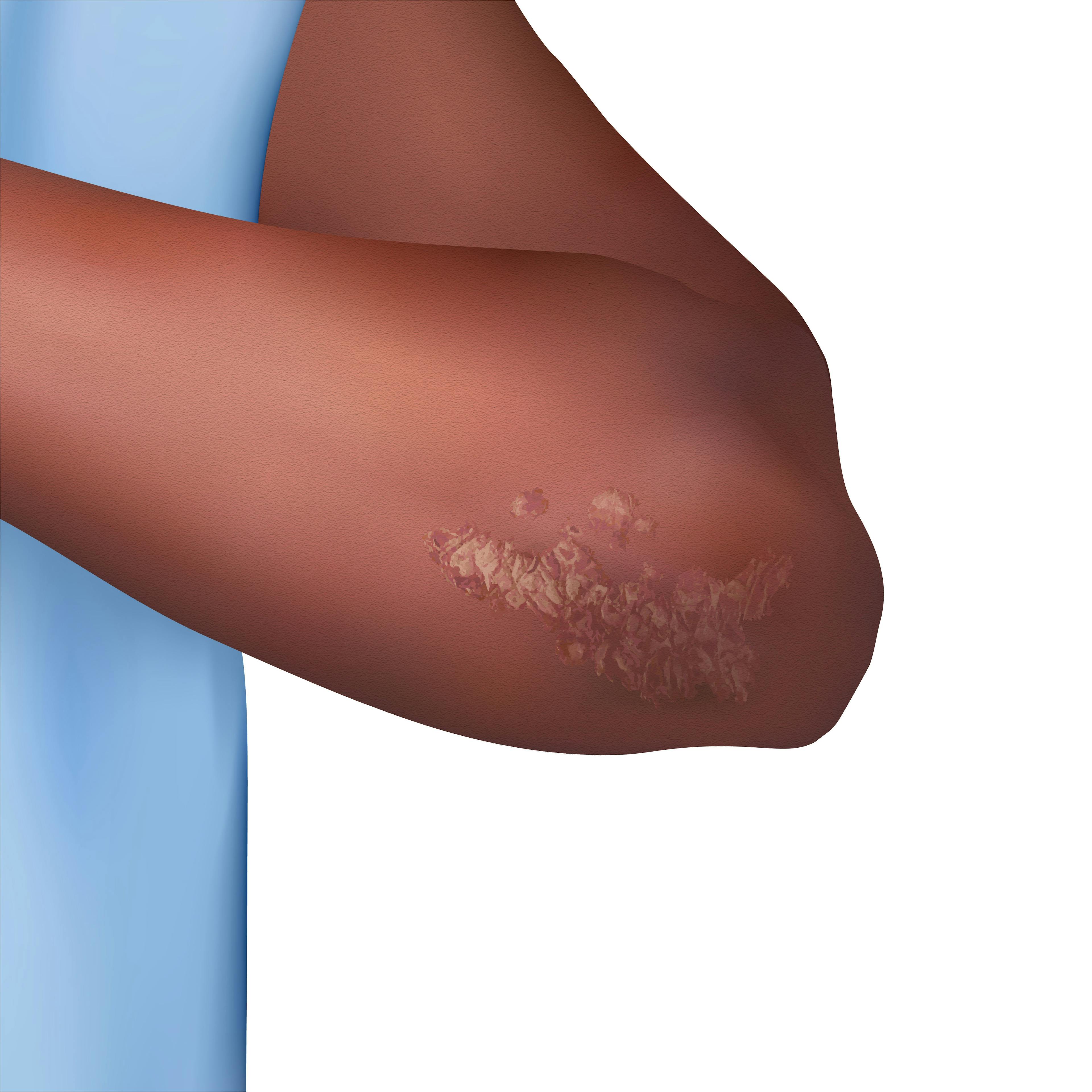
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Feature
Article
Dermatology Times
Journal Digest: August 15
Author(s):
This week’s collection of the latest dermatologic studies covers distinguishing between granular cell tumors and melanoma, methotrexate and biologics for anxiety and depression among PsO patients, botulinum toxin for scalp conditions, and a review of the SPRING study for guselkumab.
Journal of Cutaneous Pathology: Utility of Sequencing for ATP6AP1 and ATP6AP2 to Distinguish Between Atypical Granular Cell Tumor WithJunctional Component and Melanoma
According to Warren et al, a granular cell tumor (GCT) is an S100+ neoplasm with atypical and malignant variants. GCTs make nests and can have junctional components similar to melanocytic neoplasms, causing a differential diagnosis of melanoma.MelanA can be used to differentiate melanocytic from granular cell lineage, but “increasingly MelanA/SOX10 negative melanomas have been recognized by correlation with molecular methods.” Warren et al reviewed 2 cases of morphologic overlap between melanoma and atypical GCT which required additional molecular workups. From their 2 cases, Warren et al concluded that frameshift and premature stop codons in ATP6AP1/2 are specific for granular cell lineage, and capable of excluding melanoma, in the absence of known melanoma-associated driver mutations.
Indian Journal of Dermatology: The Effects of Methotrexate and Biologics on the Symptoms of Depression and Anxiety in Patients With Psoriasis
Ugurer et al compared the effects of methotrexate and biologics for psoriasis on psychiatric comorbidities among 60 patients. At baseline and 24 weeks, patients completed the Beck Anxiety Inventory (BAI), Beck Depression Inventory (BDI), and the Dermatology Life Quality Index (DLQI). The patient’s inflammation was also assessed with serum C-reactive protein and tumor necrosis factor-alpha levels. Ugurer et al found that the decrease in BAI and BDI scores at week 24 was significant in both groups, but there were no significant differences between the groups. Additionally, the decrease in DLQI scores of the patients who received biologics was significantly superior compared to the patients who received methotrexate. The authors concluded that biologics and methotrexate may reduce the symptoms of depression and anxiety among patients with psoriasis.
Dermatologic Surgery: Botulinum Toxin for Scalp Conditions: A Systematic Review
To better understand how botulinum toxin (BTX) is used in the treatment of scalp conditions, Nguyen et al performed a systematic review using PubMed/MEDLINE and Scopus and searched for the term “hair” or “scalp” along with BTX-related search terms. Articles that were selected were published before November 1, 2022, and described patients who received BTX injections for the management of scalp conditions. In total, 24 articles were identified that described 309 patients with a scalp condition treated by BTX. Androgenetic alopecia, craniofacial hyperhidrosis, and scalp hyperseborrhea had the most robust data. Nguyen et al concluded that BTX may be a potential therapy for various scalp conditions, but more studies are needed.
Journal of the European Academy of Dermatology and Venereology: Persistence and Effectiveness of Guselkumab Treatment in Patients With Moderate-to-Severe Plaque Psoriasis in a Non-Interventional Real-World Setting: The SPRING Study
The SPRING study assessed the persistence, effectiveness, and safety of guselkumab in patients with moderate-to-severe psoriasis in Spain. The phase 4, retrospective, non-interventional study had a primary endpoint of persistence (non-persistence: discontinuation or interruption ≥90 days), effectiveness was assessed using PASI and IGA scores, and DLQI and safety were also evaluated. Out of 284 patients, the 1-year probability of persistence was 89.6% and the 1-year probability of persistence was 91.9% in patients receiving guselkumab according to the Summary of Product Characteristics and 89.3% in patients with lengthened intervals of administration. After one year, PASI 90 was achieved by 56.4% of patients, IGA 0/1 response and BSA <3% were achieved by 65.5% and 77.8% of patients, respectively, and 65.8% achieved a minimal clinically significant difference (>4-point reduction) in the DLQI score at one year.
What new studies are most important to you? Share with us by emailing our team at DTEditor@mmhgroup.com.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.