- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
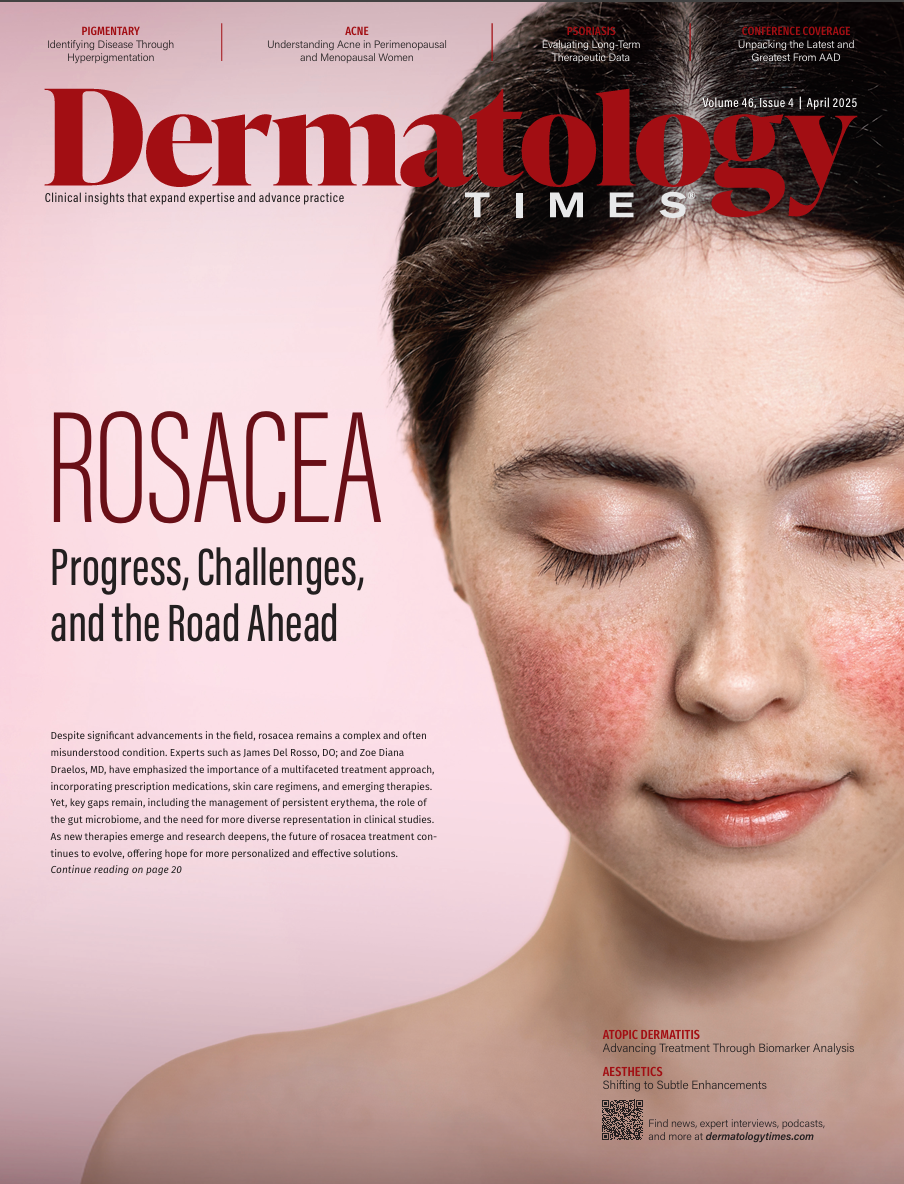
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
News
Article
Dermatology Times
Journal Digest: March 19
Author(s):
Key Takeaways
- A dermatology service-learning program for medical students improves clinical skills and supports underserved communities, with strong student satisfaction and social justice motivations.
- Blastic plasmacytoid dendritic cell neoplasm presents diagnostic challenges; early suspicion and biopsy are crucial for elderly patients with hemorrhagic lesions.
This review of the latest dermatologic studies includes insights into supporting laser tattoo removal for adults impacted by the justice-system, a case of blastic plasmacytoid dendritic cell neoplasm, and more.

Lasers in Surgery and Medicine: A protocol for dermatology service learning for medical students: supporting laser tattoo removal for adults impacted by the justice-system
A recent study explored a novel dermatology-based service-learning program designed to integrate medical students into a laser tattoo removal clinic serving individuals impacted by the criminal justice system. The program aimed to provide early clinical exposure, enhance communication skills with diverse patient populations, and foster mentorship between students while allowing participation in dermatologic care. Evaluation of the program’s first 2 cohorts indicated strong student satisfaction, with participants citing motivations rooted in social justice and interest in dermatology. Findings suggest that the initiative successfully supports students’ professional development and preparedness to serve underserved communities, though improvements in onboarding processes were noted.1
Case Reports in Dermatological Medicine: Petechiae and a persistent violaceous nodule: A presentation of blastic plasmacytoid dendritic cell neoplasm to dermatology
A recent case study discussed a rare presentation of blastic plasmacytoid dendritic cell neoplasm (BPDCN) in a 76-year-old male, characterized by erythematous macules, petechiae, purpura, and a violaceous nodule. BPDCN, a highly aggressive hematologic malignancy, often manifests with cutaneous symptoms, but its diagnosis can be challenging due to its rarity and variable presentation. The case highlights the importance of early suspicion and tissue biopsy, which led to a definitive diagnosis through immunohistochemical staining. The study emphasizes the need for dermatologists to consider BPDCN in elderly patients with hemorrhagic lesions, as early detection is critical for improving patient outcomes.2
Journal of Cosmetic Dermatology: The addition of low-dose lidocaine and triamcinolone reduces the adverse effects of 2-deoxycholate injection without affecting the long-term results
A recent study investigated the combination of low-dose triamcinolone acetonide (TAC) and lidocaine with deoxycholic acid (DCA) injections to reduce adverse effects while maintaining treatment efficacy. In a randomized trial with 15 participants, the intervention group (DCA with TAC and lidocaine) experienced significantly less pain and swelling compared to the control group (DCA with lidocaine). Both groups showed similar effectiveness in reducing submental fat, but the intervention group had a greater volumetric loss. The study concluded that the addition of TAC and lidocaine enhances patient comfort and treatment results without increasing steroid-related adverse effects.3
Journal of the European Academy of Dermatology and Venereology: Completed suicide in patients with skin disease: A systematic review and meta-analysis
A recent meta-analysis explored the risk of completed suicide in adult patients with various skin diseases. The study reviewed 37 original studies, including over 3.8 million patients, to assess the relationship between skin diseases and suicide. The findings showed no significant association between psoriasis, dermatitis, and completed suicide. However, melanoma was associated with a higher risk of suicide, with a standardized mortality rate (SMR) of 2.89, and non-melanoma skin cancer in females also showed an increased risk (SMR: 1.30). Additionally, hidradenitis suppurativa (HS) was strongly linked to an elevated suicide risk (odds ratio: 2.86). The study suggests that dermatologists should consider suicidality, particularly in patients with melanoma and HS, while further research is needed for other skin diseases.4
International Journal of Dermatology: Neutrophil extracellular traps are widely distributed across lesional and perilesional hidradenitis suppurativa skin, and elevated serum NET markers associate with moderate to severe HS disease
A recent study explored the role of neutrophil extracellular traps (NETs) in HS. The study found increased levels of CitH3, a key NET component, in both lesional and perilesional skin of patients with HS. Elevated serum levels of NET markers, including CitH3, nucleosomes, and calprotectin, were also observed in HS patients compared to healthy individuals. Additionally, higher NET marker levels correlated with more severe disease activity.5
References
- Ojeda VD, Nguyen HA, Nandamuri S, et al. A protocol for dermatology service learning for medical students: supporting laser tattoo removal for adults impacted by the justice-system. Lasers Surg Med. Published online March 11, 2025. doi:10.1002/lsm.70005
- Anzelc M, Druskovich C, Cusick A, Franklin M. Petechiae and a persistent violaceous nodule: A presentation of blastic plasmacytoid dendritic cell neoplasm to dermatology. Case Rep Dermatol Med. 2025;2025:8628105. doi:10.1155/crdm/8628105
- Ge S, Weiss RA, Schilling L, Noell CM. The addition of low-dose lidocaine and triamcinolone reduces the adverse effects of 2-deoxycholate injection without affecting the long-term results. J Cosmet Dermatol. 2025;24(3):e70072. doi:10.1111/jocd.70072
- Hrvatin Stancic B, Henning MAS, Eriksen N, Dornonville de la Cour JE, Saunte DML, Jemec GBE. Completed suicide in patients with skin disease: A systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2025;39(3):459-470. doi:10.1111/jdv.20609
- van Dalen SCM, Stein JWJ, Bruurmijn T, et al. Neutrophil extracellular traps are widely distributed across lesional and perilesional hidradenitis suppurativa skin, and elevated serum NET markers associate with moderate to severe HS disease. Int J Dermatol. Published online March 13, 2025. doi:10.1111/ijd.17706
What new studies have you been involved with or authored? Share with us by emailing DTEditor@mmhgroup.com for an opportunity to be featured.
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.



























