- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
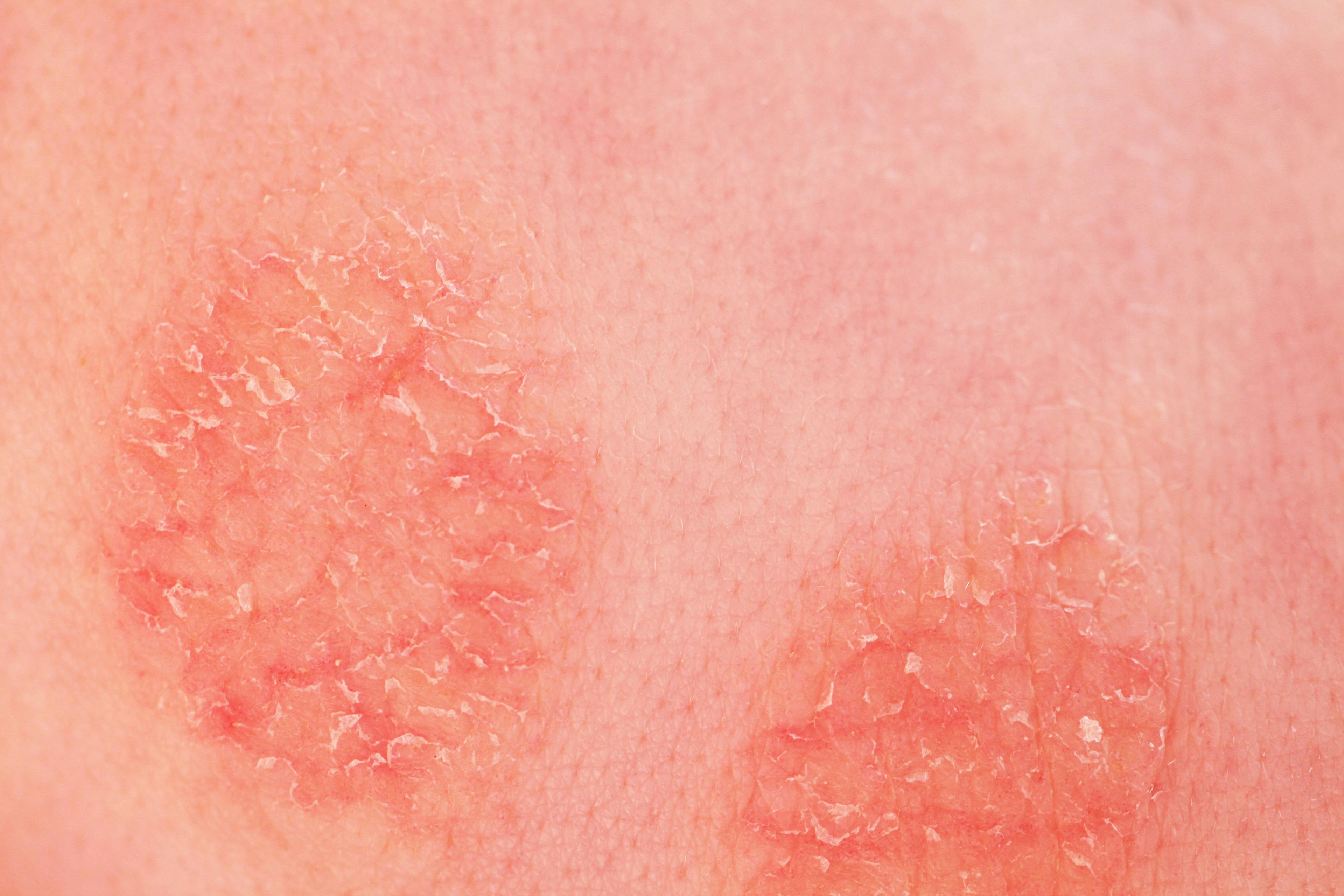
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Mental Health Affects Psoriatic Arthritis Treatment
Author(s):
Patients with anxiety/depression and psoriatic arthritis (PsA) are much less likely to achieve long-term remission. Mental health comorbidities need to be a more important part of PsA treatment.
Symptoms of anxiety and depression significantly reduce the likelihood of achieving sustained minimal disease activity (MDA) in patients with psoriatic arthritis (PsA), according to a prospective study in the journal Arthritis Care & Research.1
As a result, comprehensive management of PsA should include strategies to remedy mental health.
“We always struggle getting patients into remission with treatment for PsA,” said principal investigator Vinod Chandran, MD, PhD, DM, MBBS, a rheumatologist and clinician-scientist, is an associate professor at the University of Toronto in Ontario, Canada, an affiliate scientist with the Krembil Research Institute, a staff physician at the University Health Network and Mount Sinai Hospitals, and an associate member of the graduate faculty at the Institute of Medical Science and the Department of Laboratory Medicine and Pathobiology at the University of Toronto. He co-directs the Psoriatic Arthritis Program at the University Health Network in Toronto.
“Although we have many immunomodulatory treatments for PsA, there are other factors that also influence treatment response and the ability to achieve remission,” he said.
The current study was designed to evaluate whether mental health—mainly depression and anxiety—affects treatment response for PsA, specifically, remission or MDA.
“Mental health is less investigated than physical health among the comorbidities associated with PsA, even though it is an issue that many patients mention during clinic visits,” Chandran told Dermatology Times®.
The study comprised 743 adult patients with PsA who were treated for the condition at the University of Toronto Psoriatic Arthritis Clinic between 2008 and 2017.
Because the investigators did not personally diagnose patients for depression or anxiety, the presence of depression/anxiety fell under one of three definitions: (1) a score of ≤ 38 on the mental component summary of the 36-Item Short Form Health Survey (SF-36); (2) a score of ≤ 56 on the mental health subscale of the SF-36; and (3) a rheumatologist’s report of the diagnosis of depression/anxiety made by the patient’s family physician or psychiatrist, or pharmacotherapy for depression/anxiety, as recorded in the PsA clinic protocol.
The percentage of patients identified as having depression/anxiety at their first visit was 44.54% for the first definition, 48.99% for the second definition, and 28.4% for the third definition.
Overall, 45.36% of the entire cohort failed to achieve sustained MDA.
Specifically, the presence of depression/anxiety reduced the probability of achieving sustained MDA by 70% with the first definition, by 66% with the second definition, and by 53% with the third definition.
Two other variables independently associated with a reduced probability of achieving sustained MDA were the Charlson Comorbidity Index and the presence of fibromyalgia. Interestingly, though, daily alcohol consumption was linked to a higher probability of achieving sustained MDA.
The study, however, did not evaluate whether more severe symptoms of PsA were associated with higher rates of depression/anxiety. But the effect of depression/anxiety was independent of other comorbidities and disease severity as measured by the number of damaged joints or medications taken.
“In general, the results were expected,” Chandran said. “One of the outcomes we look at for PsA remission is pain, which correlates strongly with mental health. Similar findings have been reported in Europe.”
Chandran said patients with other inflammatory diseases are also more prone to anxiety/depression. “Some studies have looked at treating depression with biologic agents, although the results have been mixed,” he said.
“But mental health also needs to be managed in a multidisciplinary fashion,” Chandran said. “This may be less of a challenge earlier in the disease state; however, when the disease is present for some time, mental health becomes problematic because of persistent inflammation and chronic pain. The inflammation and the pain are probably driving depression/anxiety. So early control of pain might reduce the burden of these mental health issues.”
Conversely, by treating the depression/anxiety, pain is better managed, according to Chandran.
The presence of depression/anxiety may lead not only to increased sensitivity to pain, but also to avoidance, inactivity, deconditioning, and social isolation, thus contributing to a reduced likelihood of achieving remission.
Because of the high prevalence of mental health challenges among patients with PsA, Chandran firmly believes that a comprehensive evaluation needs to include a proper assessment of mental health. He conceded, though, that evaluating for mental health is difficult to integrate into clinical practice.
One alternative solution is online mindfulness-based interventions. “Also, in addition to a rheumatologist evaluating a patient, the patient might be seen by another clinician like a psychologist or even a nurse with expertise in mental health,” Chandran said.
Disclosure:
Chandran reports no relevant financial disclosures.
Reference:
1. Wong A, Ye JY, Cook RJ, Gladman DD, Chandran V. Depression and anxiety reduce the probability of achieving a state of sustained minimal disease activity in patients with psoriatic arthritis. Arthritis Care Res. Published online March 4, 2021. doi:10.1002/acr.24593
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.