- Acne
- Actinic Keratosis
- Aesthetics
- Alopecia
- Atopic Dermatitis
- Buy-and-Bill
- COVID-19
- Case-Based Roundtable
- Chronic Hand Eczema
- Chronic Spontaneous Urticaria
- Drug Watch
- Eczema
- General Dermatology
- Hidradenitis Suppurativa
- Melasma
- NP and PA
- Pediatric Dermatology
- Pigmentary Disorders
- Practice Management
- Precision Medicine and Biologics
- Prurigo Nodularis
- Psoriasis
- Psoriatic Arthritis
- Rare Disease
- Rosacea
- Skin Cancer
- Vitiligo
- Wound Care
Publication
Article
Dermatology Times
Ruxolitinib Offers Rapid Pruritus Reduction
Author(s):
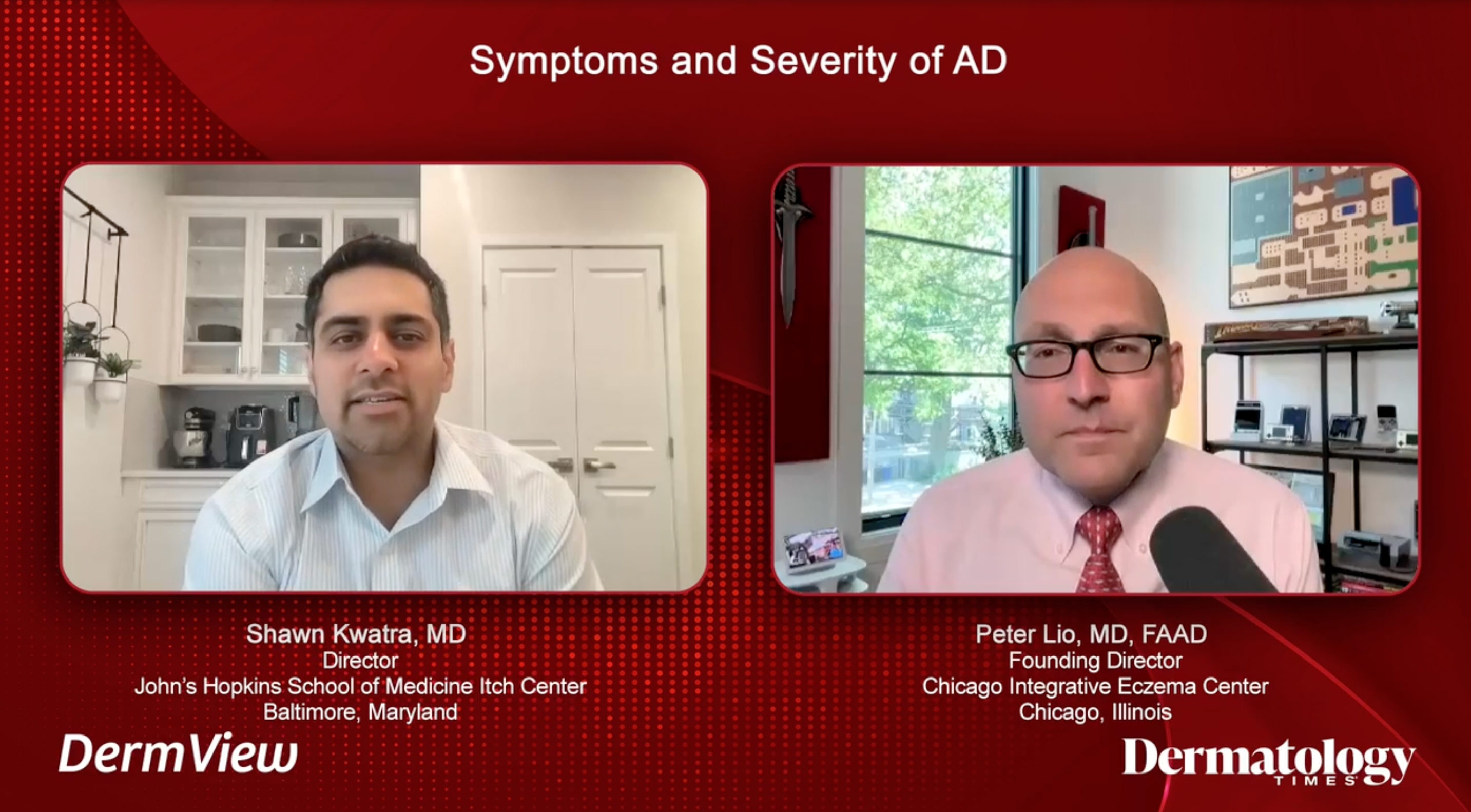
Clinicians James Q. Del Rosso, DO; Raj Chovatiya, MD, PhD; and Lisa Swanson, MD, PhD, review the study, “Rapid Pruritus Reduction With Ruxolitinib Cream in Patients With Atopic Dermatitis."
Ruxolitinib (Opzelura; Incyte) cream is a topical Janus kinase inhibitor that was approved by the US Food and Drug Administration for the treatment of atopic dermatitis (AD) in September 2021. To discuss the effects of ruxolitinib cream in reducing pruritus in patients with AD, clinicians James Q. Del Rosso, DO; Raj Chovatiya, MD, PhD; and Lisa Swanson, MD, PhD, reviewed the study, “Rapid Pruritus Reduction With Ruxolitinib Cream in Patients With Atopic Dermatitis” in Between the Lines,1 a Dermatology Times custom series.

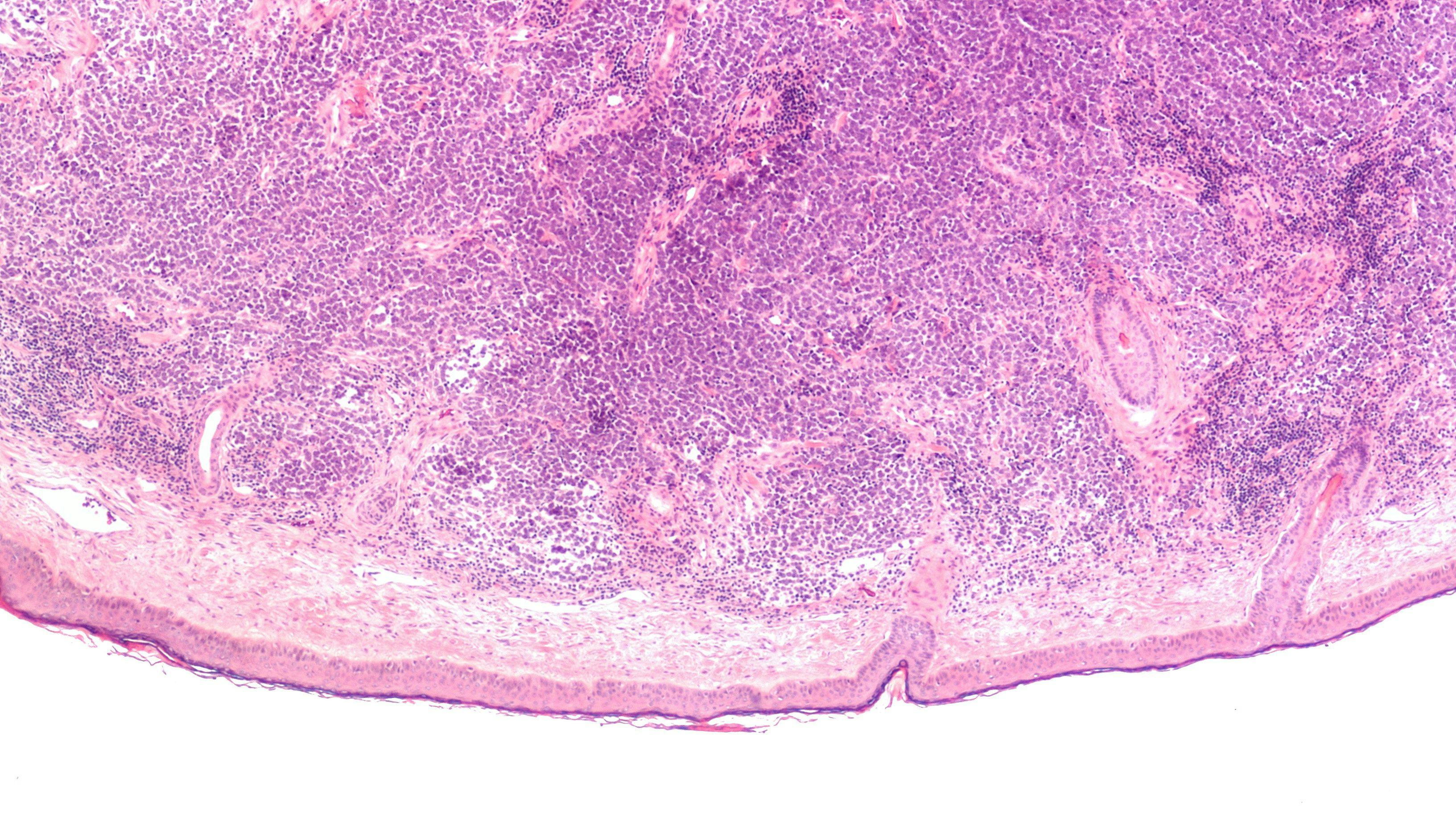
The TRuE-AD1 and TRuE-AD2 phase 3 trials,2 published in the Journal of the European Academy of Dermatology and Venereology, sought to report the timing and magnitude of pruritus reduction in AD. Researchers referenced prior studies identifying itch as the single most burdensome symptom and financial cost burden associated with AD in pediatric through adult patients.
Del Rosso began the conversation by emphasizing the chronic nature of AD, which often starts in childhood and flares on and off, affecting patients and their families daily. Despite this, Del Rosso said the impact of promising treatments on itch reduction have been less than ideal.
“We’ve had a lot of therapies for atopic dermatitis, both topical and systemic, but sometimes the effect on itch may not be quite as much as what the patient would like, especially early on,” he said.
The trials enrolled patients 12 years and older with an AD diagnosis for 2 or more years. Patients were required to present with an Investigator’s Global Assessment score of 2 or3 and a body surface area involvement of 3% to 20%, excluding the scalp. They were excluded from participation if investigators determined their AD had an unstable course or if they had other types of eczema, were immunocompromised, or had used AD treatment during either the pretrial washout period or during the study itself. A total of 1249 patients were enrolled in the study, with 1208 participating in the efficacy analysis.
Participants were randomized and treated for 8 weeks, with 483 receiving a 0.75% ruxolitinib cream, 481 receiving a 1.5% ruxolitinib cream, and 244 receiving a vehicle treatment.
“For the week between screening and going into the baseline, the subjects are given a diary and they rate each day on a scale of0 to 10, so it’s an 11-point scale going 0 to 10,” Del Rosso said. “Zero means they had no itching at all, and 10 is the worst possible itch that they could experience. Then they pick a number in between. At the end of that week, those numbers are added up and you come in with the mean or the average score. They would’ve had a report at least 4 days during that 7. If it was less than that, their data [were] not included. This gives you an assessment of how severe their itching is. You can see here it’s about a 5, which is fairly significant itching.”
Chovatiya then asked colleagues their views on using itch reduction as an end point in clinical trials.
“It’s very important because itch improvement is happiness elevation,” Swanson said. “There’s an inverse relationship between itch and happiness. The less itch you have, the more happiness you’re going to have. That’s very meaningful to me.”
Regarding itch as a trial end point, Chovatiya agreed that measuring itch, given its burden on patients, is significant.
“There’s a huge burden,” he said. “Everybody wants their itch gone yesterday. Speed is an important part in addition to magnitude. Individuals had atopic dermatitis for a long time. You weren’t dealing with the population that was just diagnosed. There’s a long existence of the disease.”
Clinicians also discussed the demographic and disease-specific data of the trial participants, noting that the location of eczematous involvement is crucial when considering treatment options for patients with AD.
“One thing that’s important to assess is facial involvement, which is very common in atopic dermatitis. Having eczematous dermatitis—red, itchy, scaly skin—on your face is obviously not something individuals like, so they scratch it,” Del Rosso said. “Facial involvement is significant. With some topical medications, we have concerns, and there are limitations on the face. About 4 of 10 patients in the study had facial involvement, and they could use the vehicle cream or the ruxolitinib cream. They didn’t know which one they were using. They could use it on the face, including the eyelids.”
As a result of the study, researchers found that 80% of participants receiving either dose of ruxolitinib cream experienced significant itch reduction at week compared to 48% of participants receiving the vehicle cream. On average, baseline itch reduction was significantly reduced among participants receiving ruxolitinib cream by week 8.
Swanson noted that of the patients enrolled in the trials, participants’ baseline characteristics were reflective of her practice: patients with mild to moderate disease with related itch who had experienced the condition for a long period of time.
“I have found that topical ruxolitinib works with the speed of a topical steroid without being a topical steroid,” she said, discussing her own practice. “And that’s one of my favorite things about it, is the rapid onset of action, rapid onset of relief for the patient.”
Chovatiya agreed, noting that both the patient demographics and data involved in the study were reflective of his own patients and their feedback.
The clinicians concluded their discussion by emphasizing the effects of ruxolitinib cream and the speed and magnitude of its results in AD-related pruritus.
“We now have a topical therapy that has not only an effect that crosses the boxes of regulatory end points but one where we can start thinking about how fast can this get working for anybody and really how something can get you to the point where I can say the majority of people are hitting all the things that we’re measuring,” Chovatiya said. “And it really makes that clinical discussion that much easier.”
References
- Del Rosso JQ, Chovatiya R, Swanson L. Dermatology Times Between The Lines. Rapid pruritus reduction with ruxolitinib cream treatment in patients with atopic dermatitis. March 30, 2023. Accessed June 1, 2023. https://www.dermatologytimes.com/view/overview-of-atopic-dermatitis
- Blauvelt A, Kircik L, Papp KA, et al. Rapid pruritus reduction with ruxolitinib cream treatment in patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2023;37(1):137-146. doi:10.1111/jdv.18571
Newsletter
Like what you’re reading? Subscribe to Dermatology Times for weekly updates on therapies, innovations, and real-world practice tips.